Volume 11, Issue 2 (6-2022)
JCHR 2022, 11(2): 137-141 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Taheri Soodejani M, Hosseini S, Sefidkar R, Madadizadeh F, Fallahzadeh H, Dehghan A, et al . Comorbidity and its Impact on Mortality of COVID-19 in Yazd Province, a Central Part of Iran: a Hospital-Based Study. JCHR 2022; 11 (2) :137-141
URL: http://jhr.ssu.ac.ir/article-1-894-en.html
URL: http://jhr.ssu.ac.ir/article-1-894-en.html
Moslem Taheri Soodejani1 
 , Saeed Hosseini2
, Saeed Hosseini2 
 , Reyhane Sefidkar1
, Reyhane Sefidkar1 
 , Farzan Madadizadeh1
, Farzan Madadizadeh1 
 , Hossein Fallahzadeh1
, Hossein Fallahzadeh1 
 , Ahmad Dehghan3
, Ahmad Dehghan3 
 , Neda Dehghani Tafti3
, Neda Dehghani Tafti3 
 , Mohammad Hassan Lotfi *4
, Mohammad Hassan Lotfi *4 


 , Saeed Hosseini2
, Saeed Hosseini2 
 , Reyhane Sefidkar1
, Reyhane Sefidkar1 
 , Farzan Madadizadeh1
, Farzan Madadizadeh1 
 , Hossein Fallahzadeh1
, Hossein Fallahzadeh1 
 , Ahmad Dehghan3
, Ahmad Dehghan3 
 , Neda Dehghani Tafti3
, Neda Dehghani Tafti3 
 , Mohammad Hassan Lotfi *4
, Mohammad Hassan Lotfi *4 

1- Center for Healthcare Data Modeling, Department of Biostatistics and Epidemiology, School of public health, ShahidSadoughi University of Medical Sciences, Yazd, Iran
2- Center for Healthcare Data Modeling, Department of Biostatistics and Epidemiology, School of public health, Shahid Sadoughi University of Medical Sciences, Yazd, Iran Department of Epidemiology, School of Public Health, Iran University of Medical Sciences, Tehran, Iran
3- Accident prevention and crisis research center, emergency organization, ShahidSadoughi University of Medical Sciences, Yazd, Iran
4- Center for Healthcare Data Modeling, Department of Biostatistics and Epidemiology, School of public health, ShahidSadoughi University of Medical Sciences, Yazd, Iran ,mhlotfi56359@gmail.com
2- Center for Healthcare Data Modeling, Department of Biostatistics and Epidemiology, School of public health, Shahid Sadoughi University of Medical Sciences, Yazd, Iran Department of Epidemiology, School of Public Health, Iran University of Medical Sciences, Tehran, Iran
3- Accident prevention and crisis research center, emergency organization, ShahidSadoughi University of Medical Sciences, Yazd, Iran
4- Center for Healthcare Data Modeling, Department of Biostatistics and Epidemiology, School of public health, ShahidSadoughi University of Medical Sciences, Yazd, Iran ,
Full-Text [PDF 90 kb]
(851 Downloads)
| Abstract (HTML) (2633 Views)
Full-Text: (468 Views)
Abstract
Introduction: The World Health Organization on March 11, 2020 declared the outbreak of severe acute respiratory syndrome Corona virus 2 disease (COVID-19) a pandemic situation. The main aim of this study was investigating mortality of COVID-19 by considering chronic diseases.
methods: This study was conducted as a cross-sectional in which all confirmed cases were examined. The variables considered in this study were age, sex, diabetes mellitus, cancers, hypertension, heart diseases, kidney diseases, and liver diseases. Independent sample t test, Chi-square and binary logistic regression were used for data analysis. All statistical analysis was done in SPSS 16 and significant level was set at 0.05.
Results: Out of 22849 PCR and CT scan tests, 16061 were positive. According to the confirmed cases, prevalence of COVID-19 was calculated about 0.019. Also hospital case fatality rate and mortality rate were calculated 156 and about 8.2 per 100000 respectively. Hypertension, and age had significant relationship with morbidity of COVID-19, in other hand, age (OR: 4.51, p<0.001), kidney diseases (OR: 1.84, p<0.001), diabetes mellitus (OR: 1.31, p<0.001), cancer (OR: 2.73, p<0.001), liver diseases (OR: 2.27, p<0.001) had impact on mortality of covid-19. Population Attributable Fraction (PAF) showed the most fraction of death was due to diabetes mellitus, cancers, kidney diseases, and liver diseases.
Conclusion: Age and some underlying diseases increase odds of death due to COVID-19. It seems that preventing high-risk people from being infected is an effective solution to reduce COVID-19 death rate. To do this, health protocols need to be implemented more seriously for these sensitive groups.
Keywords: SARS-COV-2, Risk Factors, Population attributable fraction, pandemic, Yazd, Iran
According to the latest results, the clinical symptoms of COVID-19 are heterogeneous. At the admission, 20–51% of patients have at least one co-morbidity (diabetes (10–20%); hypertension (10–15%); other cardiovascular and cerebrovascular diseases (7–40%) (4).
Thirty nine percent patients in severe disease group and twenty-one percent patients in non-severe group have previous coexisting illness (5). Co-occurrence of non-communicable diseases such as diabetes, cardiovascular disease, cancer, hypertension, kidney disease, and other chronic diseases is taken as a proven risk factor for increasing risk of acute outcome or even death from COVID-19 (6, 7). Treatment of COVID-19 in patients with underlying co-morbidity may be associated with intensive cares and ventilator supports (4). Identifying risk factors for mortality is an important component for COVID-19 management strategies. These evidences are important at a time when demand for intensive care is increasing and resources are limited (8-10).
Non-communicable diseases have been the leading causes of death in Iran in recent years so that, more than 76% of deaths are due to non-communicable diseases in Iran. Cardiovascular diseases accounted for 45.7%, cancers for 13.5% and respiratory diseases for about 4% of deaths (11). On February 19, 2020, the first cases of corona virus disease were detected in Iran (12). Based on the article by Peykari & et al., patients with at least one co-morbidity were 30.2% and the percent of death due to COVID-19 that had at least one co-morbidity was 37.9% (13).
Due to high prevalence of some chronic diseases in Yazd province, this study was designed to investigate deaths related to COVID-19 by considering chronic diseases such as diabetes, malignancies, hypertension, kidney disease and cardiovascular disease.
Methods
Data source and data extraction
All suspected cases of COVID-19 would be referred to central hospitals in order to get confirmed through PCR or CT scan test. The data have been recorded in the data registry. After making the necessary arrangements, all data included suspected, confirmed, recovered cases and deaths due to COVID-19 became available.
Study Design
In this analytical cross-sectional study, all people who had test were included. In the next step, all people were divided in two groups, including confirmed cases with Covid-19 and not confirmed cases. The variables considered in this study were age, sex, diabetes mellitus, cancers, hypertension, heart diseases, kidney diseases, and liver diseases.
Statistical analysis
Frequency (percentage), mean (SD) were used for description. Independent sample t test, Chi-square and binary logistic regression were used for data analysis. Also, population attribute fraction was estimated using the prevalence and the odds ratio of these risk factors among the control group (Eq.1).
Population attribute fraction =
( Eq .1)
In this formula OR indicates odds ratio adjusted for all risk factors and Pe represents associated prevalence risk factors in control group. All statistical analysis was done in SPSS 16 and significant level was set at 0.05.
Results
Out of 22849 PCR and CT scan tests, 16061 were positive. According to the confirmed cases, prevalence of COVID-19 was about 0.019. Also hospital case fatality rate and mortality rate were 156 and about 8.2 per 100000, respectively.
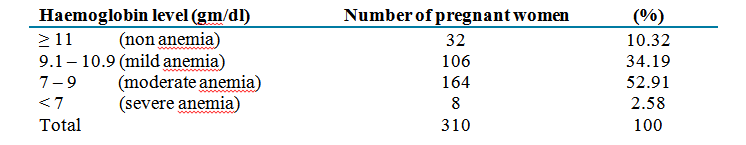
Mean (SD) of age between confirmed cases and nit confirmed cases were significantly different (p<0.001); also, some of chronic diseases such as diabetes mellitus and hypertension were shown to be associated with result of COVID-19 test (p<0.05) (table1).
Results of univariate logistic regression demonstrated that some of chronic diseases could increase the odds of death due to covid-19, but after adjustment for age and other chronic diseases, it was observed that diabetes mellitus, kidney diseases and cancers significantly increased this odds (p<0.05) (table2).
Prevalence of diabetes mellitus, liver diseases, kidney diseases, and cancers were calculated 14.4%, 0.19 %, 1.66%, and 1.46% respectively. The PAF of these chronic diseases are reported in table2.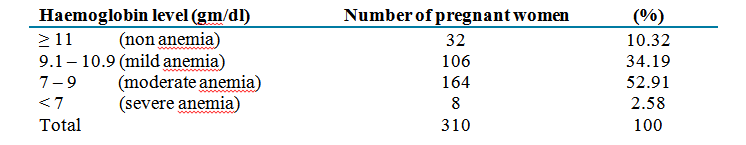

Introduction: The World Health Organization on March 11, 2020 declared the outbreak of severe acute respiratory syndrome Corona virus 2 disease (COVID-19) a pandemic situation. The main aim of this study was investigating mortality of COVID-19 by considering chronic diseases.
methods: This study was conducted as a cross-sectional in which all confirmed cases were examined. The variables considered in this study were age, sex, diabetes mellitus, cancers, hypertension, heart diseases, kidney diseases, and liver diseases. Independent sample t test, Chi-square and binary logistic regression were used for data analysis. All statistical analysis was done in SPSS 16 and significant level was set at 0.05.
Results: Out of 22849 PCR and CT scan tests, 16061 were positive. According to the confirmed cases, prevalence of COVID-19 was calculated about 0.019. Also hospital case fatality rate and mortality rate were calculated 156 and about 8.2 per 100000 respectively. Hypertension, and age had significant relationship with morbidity of COVID-19, in other hand, age (OR: 4.51, p<0.001), kidney diseases (OR: 1.84, p<0.001), diabetes mellitus (OR: 1.31, p<0.001), cancer (OR: 2.73, p<0.001), liver diseases (OR: 2.27, p<0.001) had impact on mortality of covid-19. Population Attributable Fraction (PAF) showed the most fraction of death was due to diabetes mellitus, cancers, kidney diseases, and liver diseases.
Conclusion: Age and some underlying diseases increase odds of death due to COVID-19. It seems that preventing high-risk people from being infected is an effective solution to reduce COVID-19 death rate. To do this, health protocols need to be implemented more seriously for these sensitive groups.
Keywords: SARS-COV-2, Risk Factors, Population attributable fraction, pandemic, Yazd, Iran
Introduction
The World Health Organization on March 11, 2020 declared the outbreak of severe acute respiratory syndrome Corona virus 2 disease (COVID-19) a pandemic situation(1). For the first time, COVID-19 was reported in Wuhan (Hubei Province, China) in late December(2). From the beginning of the pandemic, there have been over 79.2 million cases and over 1.7 million deaths reported(3).According to the latest results, the clinical symptoms of COVID-19 are heterogeneous. At the admission, 20–51% of patients have at least one co-morbidity (diabetes (10–20%); hypertension (10–15%); other cardiovascular and cerebrovascular diseases (7–40%) (4).
Thirty nine percent patients in severe disease group and twenty-one percent patients in non-severe group have previous coexisting illness (5). Co-occurrence of non-communicable diseases such as diabetes, cardiovascular disease, cancer, hypertension, kidney disease, and other chronic diseases is taken as a proven risk factor for increasing risk of acute outcome or even death from COVID-19 (6, 7). Treatment of COVID-19 in patients with underlying co-morbidity may be associated with intensive cares and ventilator supports (4). Identifying risk factors for mortality is an important component for COVID-19 management strategies. These evidences are important at a time when demand for intensive care is increasing and resources are limited (8-10).
Non-communicable diseases have been the leading causes of death in Iran in recent years so that, more than 76% of deaths are due to non-communicable diseases in Iran. Cardiovascular diseases accounted for 45.7%, cancers for 13.5% and respiratory diseases for about 4% of deaths (11). On February 19, 2020, the first cases of corona virus disease were detected in Iran (12). Based on the article by Peykari & et al., patients with at least one co-morbidity were 30.2% and the percent of death due to COVID-19 that had at least one co-morbidity was 37.9% (13).
Due to high prevalence of some chronic diseases in Yazd province, this study was designed to investigate deaths related to COVID-19 by considering chronic diseases such as diabetes, malignancies, hypertension, kidney disease and cardiovascular disease.
Methods
Data source and data extraction
All suspected cases of COVID-19 would be referred to central hospitals in order to get confirmed through PCR or CT scan test. The data have been recorded in the data registry. After making the necessary arrangements, all data included suspected, confirmed, recovered cases and deaths due to COVID-19 became available.
Study Design
In this analytical cross-sectional study, all people who had test were included. In the next step, all people were divided in two groups, including confirmed cases with Covid-19 and not confirmed cases. The variables considered in this study were age, sex, diabetes mellitus, cancers, hypertension, heart diseases, kidney diseases, and liver diseases.
Statistical analysis
Frequency (percentage), mean (SD) were used for description. Independent sample t test, Chi-square and binary logistic regression were used for data analysis. Also, population attribute fraction was estimated using the prevalence and the odds ratio of these risk factors among the control group (Eq.1).
Population attribute fraction =
In this formula OR indicates odds ratio adjusted for all risk factors and Pe represents associated prevalence risk factors in control group. All statistical analysis was done in SPSS 16 and significant level was set at 0.05.
Results
Out of 22849 PCR and CT scan tests, 16061 were positive. According to the confirmed cases, prevalence of COVID-19 was about 0.019. Also hospital case fatality rate and mortality rate were 156 and about 8.2 per 100000, respectively.
Mean (SD) of age between confirmed cases and nit confirmed cases were significantly different (p<0.001); also, some of chronic diseases such as diabetes mellitus and hypertension were shown to be associated with result of COVID-19 test (p<0.05) (table1).
Results of univariate logistic regression demonstrated that some of chronic diseases could increase the odds of death due to covid-19, but after adjustment for age and other chronic diseases, it was observed that diabetes mellitus, kidney diseases and cancers significantly increased this odds (p<0.05) (table2).
Prevalence of diabetes mellitus, liver diseases, kidney diseases, and cancers were calculated 14.4%, 0.19 %, 1.66%, and 1.46% respectively. The PAF of these chronic diseases are reported in table2.

Discussion
The results of this study revealed that factors such as aging, diabetes, kidney disease, various types of cancer and liver disease are leading risk factors of death due to COVID-19. Age is a potential risk factor for mortality. A conducted study on the probability of death in COVID-19 patients, which were over 60 years, showed that these people were more likely to die than other age groups (14). So, it seems that age has a significant contribution to assess final outcome of COVID-19.
Diabetes is one of the most common underlying disorders with a relatively high prevalence in Yazd province. It seems that death due to COVID-19 in patients with this diabetes is significantly high. The result of a review study indicated that odds of death due to COVID-19 in people with diabetes is up to three times more than others (5).
Kidney disease is another risk factor for death from COVID-19. Our findings showed that people with kidney disease had higher odds to die than people without the disease. This result is consistent with other studies which reported that kidney disease increases odds of death up to 5 times (5).
Also, the number of deaths due to COVID-19 in people with cancer is high due to the effect that various types of cancer have on the immune system. A review study demonstrated that cancer increases odds of death of infected cases up to 3 times (15).
Chronic liver disease, which elevates the risk of death of people with the virus, can also be one of the determinant factors of the final outcome of patients with COVID-19. Several studies have also shown that people with liver disease are more vulnerable so that liver disease increases the odds of death in contaminated cases (8, 16, 17).
PAF showed that diabetes mellitus, kidney diseases, cancers, and liver diseases have most impact on death of COVID-19, which could be related to the high prevalence of the chronic diseases in Yazd province (18).
It seems that if we want to reduce the mortality of COVID-19, we should prevent morbidity of COVID-19 in people with these diseases.
The use of all recorded data related to hospitalized patients was one of the strengths of the present study. Also, this study was conducted for the first time in Yazd province, which is located in the central region of Iran. One of the limitations of this study was the lack of coverage of outpatient data.
Conclusion
According to the results of this study, various factors including age and some underlying diseases increase odds of death due to COVID-19. It seems that preventing high-risk people from being infected is an effective solution to reduce COVID-19 death rate. To do this, health protocols need to be implemented more seriously for these sensitive groups.
Conflict of interest
None.
Ethical approval
This study was presented in the ethics committee of School of Medicine affiliated to Shahid Sadoughi University of Medical Sciences, Yazd, Iran and was approved according to the approval ethical code IR.SSU.SPH.REC.1400.030.
Authors’ contributions
All authors contributed to writing,
editing, reviewing the manuscript for important
intellectual content.
The results of this study revealed that factors such as aging, diabetes, kidney disease, various types of cancer and liver disease are leading risk factors of death due to COVID-19. Age is a potential risk factor for mortality. A conducted study on the probability of death in COVID-19 patients, which were over 60 years, showed that these people were more likely to die than other age groups (14). So, it seems that age has a significant contribution to assess final outcome of COVID-19.
Diabetes is one of the most common underlying disorders with a relatively high prevalence in Yazd province. It seems that death due to COVID-19 in patients with this diabetes is significantly high. The result of a review study indicated that odds of death due to COVID-19 in people with diabetes is up to three times more than others (5).
Kidney disease is another risk factor for death from COVID-19. Our findings showed that people with kidney disease had higher odds to die than people without the disease. This result is consistent with other studies which reported that kidney disease increases odds of death up to 5 times (5).
Also, the number of deaths due to COVID-19 in people with cancer is high due to the effect that various types of cancer have on the immune system. A review study demonstrated that cancer increases odds of death of infected cases up to 3 times (15).
Chronic liver disease, which elevates the risk of death of people with the virus, can also be one of the determinant factors of the final outcome of patients with COVID-19. Several studies have also shown that people with liver disease are more vulnerable so that liver disease increases the odds of death in contaminated cases (8, 16, 17).
PAF showed that diabetes mellitus, kidney diseases, cancers, and liver diseases have most impact on death of COVID-19, which could be related to the high prevalence of the chronic diseases in Yazd province (18).
It seems that if we want to reduce the mortality of COVID-19, we should prevent morbidity of COVID-19 in people with these diseases.
The use of all recorded data related to hospitalized patients was one of the strengths of the present study. Also, this study was conducted for the first time in Yazd province, which is located in the central region of Iran. One of the limitations of this study was the lack of coverage of outpatient data.
Conclusion
According to the results of this study, various factors including age and some underlying diseases increase odds of death due to COVID-19. It seems that preventing high-risk people from being infected is an effective solution to reduce COVID-19 death rate. To do this, health protocols need to be implemented more seriously for these sensitive groups.
Conflict of interest
None.
Ethical approval
This study was presented in the ethics committee of School of Medicine affiliated to Shahid Sadoughi University of Medical Sciences, Yazd, Iran and was approved according to the approval ethical code IR.SSU.SPH.REC.1400.030.
Authors’ contributions
All authors contributed to writing,
editing, reviewing the manuscript for important
intellectual content.
Review: Research |
Subject:
Epidemiology
Received: 2022/04/20 | Accepted: 2022/06/20 | Published: 2022/07/5
Received: 2022/04/20 | Accepted: 2022/06/20 | Published: 2022/07/5
References
1. Hosseini S, Bahrevar V, Rahmanian V, Hazar N. Fear of COVID 19 Pandemic: A case study in Iran. Pakistan Journal of Medical and Health Sciences. 2020;14(2):484-7.
2. Hosseini S, Mohsenpour MA, Bahrevar V, Rahmanian V, Hazar N. Which information sources do people choose during the COVID-19 pandemic: Mass media or social media? A survey in Iran. Pakistan Journal of Medical and Health Sciences. 2020;14(3):1562-5.
3. Organization WH. Coronavirus disease ( COVID-19): weekly epidemiological update. 2020.
4. Guan W-j, Liang W-h, Zhao Y, Liang H-r, Chen Z-s, Li Y-m, et al. Comorbidity and its impact on 1590 patients with Covid-19 in China: A Nationwide Analysis. European Respiratory Journal. 2020;55(5). [DOI:10.1183/13993003.01227-2020]
5. Nandy K, Salunke A, Pathak SK, Pandey A, Doctor C, Puj K, et al. Coronavirus disease (COVID-19): A systematic review and meta-analysis to evaluate the impact of various comorbidities on serious events. Diabetes & Metabolic Syndrome: Clinical Research & Reviews. 2020;14(5):1017-25. [DOI:10.1016/j.dsx.2020.06.064]
6. Sanyaolu A, Okorie C, Marinkovic A, Patidar R, Younis K, Desai P, et al. Comorbidity and its Impact on Patients with COVID-19. SN comprehensive clinical medicine. 2020:1-8. [DOI:10.1007/s42399-020-00363-4]
7. Ye C, Zhang S, Zhang X, Cai H, Gu J, Lian J, et al. Impact of comorbidities on patients with COVID‐19: A large retrospective study in Zhejiang, China. Journal of Medical Virology. 2020;92(11):2821-9. [DOI:10.1002/jmv.26183]
8. Cho SI, Yoon S, Lee H-J. Impact of comorbidity burden on mortality in patients with COVID-19: a retrospective analysis of the Korean health insurance database. 2020. [DOI:10.21203/rs.3.rs-54298/v1]
9. Grasselli G, Zangrillo A, Zanella A, Antonelli M, Cabrini L, Castelli A, et al. Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy Region, Italy. Jama. 2020;323(16):1574-81. [DOI:10.1001/jama.2020.5394]
10. Rosenbaum L. Facing Covid-19 in Italy-ethics, logistics, and therapeutics on the epidemic's front line. New England Journal of Medicine. 2020;382(20):1873-5. [DOI:10.1056/NEJMp2005492]
11. Organization WH. Islamic Republic of Iran country health profile 2020
12. Daneshpazhooh M, Mahmoudi H. COVID-19: The experience from Iran. Clinics in Dermatology. 2020. [DOI:10.1016/j.clindermatol.2020.12.009]
13. Peykari N, Eybpoosh S, Safikhani H, Haghdoost AA, Tabatabaei-Malazy O, Larijani B. Non-communicable Diseases and COVID-19; a double-edged sword A Special Communication from IRAN. Journal of Diabetes & Metabolic Disorders. 2020:1-5. [DOI:10.1007/s40200-020-00683-1]
14. Yanez ND, Weiss NS, Romand J-A, Treggiari MM. COVID-19 mortality risk for older men and women. BMC Public Health. 2020;20(1):1-7. [DOI:10.1186/s12889-020-09826-8]
15. Tian Y, Qiu X, Wang C, Zhao J, Jiang X, Niu W, et al. Cancer associates with risk and severe events of COVID‐19: A systematic review and meta‐analysis. International journal of cancer. 2021;148(2):363-74. [DOI:10.1002/ijc.33213]
16. Wang B, Li R, Lu Z, Huang Y. Does comorbidity increase the risk of patients with COVID-19: evidence from meta-analysis. Aging (Albany NY). 2020;12(7):6049. [DOI:10.18632/aging.103000]
17. Jakhmola S, Indari O, Baral B, Kashyap D, Varshney N, Das A, et al. Comorbidity assessment is essential during COVID-19 treatment. Frontiers in physiology. 2020;11. [DOI:10.3389/fphys.2020.00984]
18. Lotfi MH, Saadati H, Afzali M. Prevalence of diabetes in people aged≥ 30 years: the results of screen-ing program of Yazd Province, Iran, in 2012. Journal of research in health sciences. 2013;14(1):88-92.
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution 4.0 International License. |