BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
URL: http://jhr.ssu.ac.ir/article-1-937-en.html


 1, Prabhakumari Chellamma2
1, Prabhakumari Chellamma2 

 , Sajna Mathumkunnath Vijayan3
, Sajna Mathumkunnath Vijayan3 

 , Jackson Kulampallil Sebastian4
, Jackson Kulampallil Sebastian4 

 , Rini Raveendran5
, Rini Raveendran5 


2- Department of Community Medicine, Travancore Medical College, Kollam, Kerala, India
3- Department of Community Medicine, Government Medical College, Idukki, Kerala, India
4- Department of General Surgery, Government Medical College, Wayanad, Kerala, India
5- Department of Community Medicine, Government Medical College, Thrissur, Kerala, India
|
|
Breastfeeding Practices among Urban Mothers of Central Kerala, India: A Cross-Sectional Study |
|
Fathimathusalma Othayoth 1*


Jackson Kulampallil Sebastian 4
-
Department of Community Medicine, Government Medical College, Kozhikode, Kerala, India
-
Department of Community Medicine, Travancore Medical College, Kollam, Kerala, India
-
Department of Community Medicine, Government Medical College, Idukki, Kerala, India
-
Department of General Surgery, Government Medical College, Wayanad, Kerala, India
-
Department of Community Medicine, Government Medical College, Thrissur, Kerala, India
|
ARTICLE INFO |
|
ABSTRACT |
|
Original Article |
|
Background: The practice of breastfeeding is vital in child nutrition and morbidity. The authors aimed to determine breastfeeding practices and factors related to Exclusive Breastfeeding (EBF) among mothers with children aged six months to 2 years in an urban area of Thrissur district, Kerala, India. Methods: This was a community-based and cross-sectional study conducted on 339 mothers using cluster sampling in 2016 for one year in the urban area of Thrissur district, Kerala. Details regarding sociodemographic factors, obstetric history, child-related data and breastfeeding practices were collected from mothers using a pretested and semi-structured questionnaire. Analyses were done using SPSS16 and Epi Info 7. Results: The mean age of study population was 27.21 ± 4.27. 223 mothers (65.78 %, 95% CI = 60.43-70.77) initiated breastfeeding within 1 hour, and prelacteal feeding was observed in 25 cases (7.37%, 95% CI = 4.92-10.83). 99.71% practiced feeding on demand, and 30.97% (95% CI = 26.15- 36.24) of children were exclusively breastfed up to 6 months with mean duration of 3.95± 1.79 months. The mean age at which complementary feeding started was 4.83±1.32 months. Cultural beliefs, mothers' employment, and problems during breastfeeding were significant predictors of EBF for up to 6months. |
|
|
||
|
|
|
|
|
|
How to cite this paper:
Othayoth F, Chellamma P, Mathumkunnath Vijayan S, Kulampallil Sebastian J, Raveendran R. Breastfeeding Practices among Urban Mothers of Central Kerala, India: A Cross-Sectional Study. J Community Health Research 2024; 13(1): 22-31.
Introduction
Breast milk is the best source of nutrition for an infant and plays a vital role in child survival. Even though breastfeeding is a common practice in India, the appropriate breastfeeding practices are not satisfactory, resulting in malnutrition among children. In 2020, it was estimated that 38.9 million children were overweight or obese, 45 million were wasted, and 149 million children under the age of five were stunted (i.e., too short for their age) (1). Breastfeeding practices are practices followed while breastfeeding a baby, and include prelacteal feeding, breastfeeding initiation, exclusive breastfeeding (EBF) for 6 months (EBF), predominant breastfeeding, bottle feeding, and timely initiation of complementary feeding (2). The World Health Organization (WHO) recommends that infants be exclusively breastfed for the first six months, followed by complementary foods until the age of 2 or above (3). The beneficial effects of breastfeeding depend on its initiation as early as possible (avoiding delay beyond an hour), duration and the age at which breastfed children are weaned (4). Several other factors like the community's educational, social, cultural, and economic factors also significantly affect the different breastfeeding practices (4). UNICEF and WHO launched Baby-Friendly Hospital Initiative in 1992 to protect, promote, and support breastfeeding (5).
The practice of prelacteal feeding, whereby infants receive food or liquid before initiating breastfeeding for the first time (2), is widespread in many Indian societies (6,7). This practice could introduce infection, sensitize the gut to foreign proteins, or delay the onset of lactation (8), resulting in harmful effects on the newborn. According to the National Family Health Survey, 46.3% of children in India are exclusively breastfed for six months of age (9). The low prevalence and duration of exclusive breastfeeding increase the risk of infant and childhood morbidity in both developed and developing countries (10). Predominant breastfeeding practices, including giving other fluids like tea, water, and sugar water in limited quantities, along with breastmilk (11), are also seen in many parts of India due to the lack of awareness. The practice of bottle feeding and feeding with infant formula is also widespread in many parts of India (12, 13). Data from various sources showed that a breastfed child has a greater chance of survival than an artificially fed child (3, 14). Continuing breastfeeding for 2 years along with EBF helps to prevent early malnutrition and is very important to achieve optimal growth and development (3).
There are a few studies conducted in Kerala regarding breastfeeding practices. Compared to other states in India, the literacy rate of Kerala is much higher, and the literacy rate in the urban areas is higher than rural area (15). Despite high literacy rate, breastfeeding practices are not improved substantially. The prevalence of EBF among infants under 6 is 55.5% (16), despite Kerala's high literacy rate of 94% (15). Moreover, most of the mothers in urban areas of Kerala are employed, and breastfeeding practices may be different. Hence, this study helps to promote appropriate breastfeeding activities in the community by assessing the different breastfeeding practices and factors associated with EBF up to six months among mothers with children of six months to 2 years in the urban area of Thrissur district, Central Kerala, India.
Methods
A community-based and cross-sectional study was conducted for one year during the year 2016, in the corporation area of Thrissur district, Kerala. Mothers with children aged 6 months to 2, residing in the area for a minimum period of 6 months, were included in the study. After obtaining written informed consent to participate in the study, an interview was conducted among mothers using the pretested semi-structured questionnaire. The authors interviewed the mothers individually, after explaining the purpose of the study and ensuring the subject's confidentiality. The study protocol was approved by the Institutional Research and Ethics Committees of Govt. Medical College, Thrissur. Consent for the study was also taken from the Mayor of the Thrissur Corporation.
Thrissur district is situated in central Kerala. Thrissur Municipal Corporation is the civic body which governs Thrissur city in Kerala. It has a population of 325474, spread over 101.42 sq. km and divided into five divisions such as Ayyanthole, Vilvattom, Ollukkara, Ollur and Koorkanchery, which was again divided into 55 wards (17). Cluster sampling technique was used in, and each ward in this corporation was considered a cluster. There were 55 wards in the corporation area of Thrissur district. Therefore, 55 wards were considered 55 clusters. 20 clusters were selected by simple random method using the lottery method. In order to achieve a required sample size of 352, 18 subjects were included from each cluster. The first subject was chosen from the first household on a randomly chosen lane at the site of arrival in the cluster, usually the main bus stop. The survey, then, proceeded to consecutive houses on either side of the road until 18 mothers were chosen. If more than one mother was present in the same household, all of them were included in the study. Houses, where the subject was absent during the visit, were revisited two more times in the subsequent days to increase the response rate.
The study was conducted for a period of one year, and data collection was completed in four months. Data included sociodemographic profile, obstetric history, infant details, and breastfeeding practices. Details of antenatal checkups, childbirth and postnatal checkups were cross-checked with their MCP card or hospital records wherever possible. The socioeconomic status of the concerned family was assessed using the modified Kuppuswamy's scale (18) for the urban population and classified accordingly.
The sample size was calculated as 352 by considering a prevalence rate of 38%, for the youngest surviving child exclusively breastfed for the first six months (19), α error of 5%, design effect as 2 ,and a 10% non-response rate. Data collected from each individual was entered into a Microsoft Excel sheet after coding and rechecking of variables. General characteristics of the sample population were described in terms of proportions. The pattern of different breastfeeding practices among the study population was measured using proportions and a confidence interval of 95%. Quantitative variables were summarized using mean duration and standard deviation. According to the nature of the covariates, factors associated with different breastfeeding practices were assessed by bivariate analyses through chi-square test or t-test. The odds ratios and their 95% confidence intervals were computed to measure the strength of the association. Regression analysis was carried out to discover determinant factors of various breastfeeding practices. The significance level was estimated with a 95% confidence interval, and analyses were done with the help of SPSS and Epi Info 7.
Results
Out of the 352 subjects eligible for the study, 339 mothers participated in the study. The overall response rate was 96.3%, and the mean age of the subjects was 27.21 ± 4.27. Among them, 78.48% of the mothers had an education above senior high school education level, and only 19.17% of the mothers were employed. The sociodemographic characteristics of the study participants are given in Table. 1
Table 1. Sociodemographic characteristics of the participants
|
Variable |
Category |
Frequency |
Percentage |
|
Age group (years ) |
11- 20 |
8 |
2.36 |
|
21- 30 |
262 |
77.29 |
|
|
31- 40 |
67 |
19.76 |
|
|
41- 50 |
2 |
0.59 |
|
|
Religion |
Hindu |
184 |
54.28 |
|
Christian |
122 |
35.99 |
|
|
Muslim |
33 |
9.73 |
|
|
Education |
Primary |
1 |
0.29 |
|
Secondary |
1 |
0.29 |
|
|
Senior secondary education(Grades 10-12) |
71 |
20.94 |
|
|
Graduated and above |
266 |
78.48 |
|
|
Occupation |
Housewife |
274 |
80.83 |
|
Professional |
11 |
3.25 |
|
|
Semiprofessionals |
21 |
6.19 |
|
|
Others |
33 |
9.73 |
|
|
Socio-economic status |
Lower |
0 |
0 |
|
Upper lower |
24 |
7.08 |
|
|
Middle/lower middle |
183 |
53.98 |
|
|
Upper middle |
115 |
33.93 |
|
|
Upper |
17 |
5.01 |
|
|
Type of family |
Nuclear |
62 |
18.29 |
|
Joint |
277 |
81.71 |
Breastfeeding practices of the participants
The distribution of different breastfeeding practices is described in Table 2.25 (7.37%) mothers gave prelacteal feeds to newborns. The common prelacteal feeds were giving Zam-zam water to (holy water from Mecca), 13 (52%) babies, 6 (24%) babies, Infant formula–lactogen, and 3 (12%) babies were fed with honey. The proportion of
Table 2. Summary of various breastfeeding practices (n = 339)
|
Variable |
Frequency |
Percentage |
95% CI |
|
Pre-lacteal feeding |
25 |
7.37 |
4.92 - 10.83 |
|
Early initiation of breastfeeding (< 1 hour) |
223 |
65.78 |
60.43 - 70.77 |
|
Colostrum feeding |
339 |
100 |
100 – 100 |
|
EBF up to 6 months |
105 |
30.97 |
26.15 - 36.24 |
|
Predominant breastfeeding before 6 months |
115 |
33.92 |
28.95 – 39.27 |
|
Complementary feeding at 6 months |
163 |
48.08 |
42.67 - 53.54 |
|
Bottle feeding |
164 |
48.38 |
42.96– 53.83 |
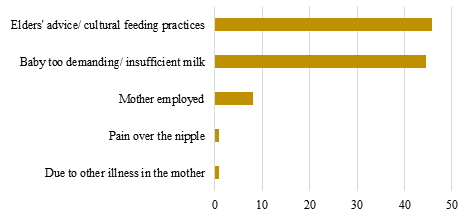
Figure 1. Reasons for early cessation of EBF (n = 234)
Benefits of EBF for 6 months
The benefits of exclusive breastfeeding in this study were assessed based on the occurrence of illness among the children during EBF period and the duration of lactational amenorrhoea (Tables 3 and 4). The odds of developing illness among those who were not exclusively breastfed until 6 months was 3.2 times higher as compared to those who were exclusively breastfed up to 6 months (OR = 3.20, 95% CI = 1.31- 7.82). The delayed return of menstrual period was observed in those mothers who practiced EBF, even though it was not significant.
Table 3. Association between illness in the child and EBF until 6 months of age
|
EBF up to 6months |
Illness present (%) |
Illness |
OR |
χ² |
P-value |
|
Not practiced |
38 |
196 |
3.20 |
7.108 |
0.007 |
|
Practiced |
6 |
99 |
|||
|
Total |
44 |
295 |
Table 4. Exclusive breastfeeding duration versus lactational amenorrhoea duration
|
EBF duration |
Lactational Amenorrhoea |
T value |
P-value |
|
< 6 months (n = 234) |
4.25 ± 2.93months |
1.687 |
0.09 |
|
≥ 6 months (n = 105) |
4.83 ± 2.92 months |
Obstetric and child details of the study participants
240 (70.80%) mothers received breastfeeding advice at antenatal checkups, and health workers conducted home visits regarding 291 (85.84%) mothers. All the deliveries were institutional, 56 of which (16.52%) occurred in government hospitals. Among the 339 mothers, 210 (61.95%) were had vaginal delivery, and the rest, 129 mothers (38.05%) underwent Caesarian sections. The mean age of children in the study was 14 ± 5.6 months and ranged from 6 months to 24 months. The majority of the children, 173 (51%), belonged to the age group 6- 12 months, 109 (32.2%) were between 12 months to 18 months, and 57 (16.8%) children were between 19 months to 24 months. Most of the children, 183 (53.98%), were females. The mean birth weight was 2.99 ± 0.48 Kg, with a minimum birth weight of 950 gm to a maximum of 4.5 kg.
Factors associated with EBF until 6 months
Cultural beliefs, mothers' employment, and problems during breastfeeding (such as insufficient milk and cracked/retracted nipple) were significant predictors of EBF until 6 months of age (Tables 5 and 6). Being above 30, religion, joint family system, educational level of senior high school and below and breastfeeding advice given by public health staff during house visits also affected EBF in the study area, even though it was not significant.
Table 5. Sociodemographic factors associated with EBF
|
Variable |
Category |
EBF up to 6 months |
Odds ratio (95% confidence interval) |
||
|
No (%) |
Yes (%) |
COR* (95% CI) |
AOR**(95% CI) |
||
|
Age |
Age ≤ 30yrs |
188 (69.6) |
82 (30.4) |
1.146 |
1.07 |
|
Age > 30 yrs |
46 (66.7) |
23 (33.3) |
|||
|
Religion |
Hindu |
134 (72.8) |
50 (27.2) |
1.74 |
1.19 |
|
Christian |
80 (65.6) |
42 (34.4) |
1.23 |
1.23 |
|
|
Muslim |
20 (60.6) |
13 (39.4) |
1 |
1 |
|
|
Type of Family |
Joint |
196 (70.8) |
81 (29.2) |
1.53 |
1.26 |
|
Nuclear |
38 (61.3) |
24 (38.7) |
|||
|
Mothers' education |
Senior secondary education and below |
122 (71.3) |
49 (28.7) |
1.245 |
1.29 |
|
Graduated and above |
112 (66.7) |
56 (33.3) |
|||
|
Mothers' occupation |
Employed |
50 (76.9) |
15 (23.1) |
1.63 |
2.01 |
|
Unemployed |
184 (67.2) |
90 (32.8) |
|||
*Crude OR, **Adjusted OR
Table 6. Cultural and maternal factors associated with EBF
|
Variable |
Category |
EBF up to 6 months |
Odds ratio (95% confidence interval) |
||
|
No (%) |
Yes (%) |
COR* |
AOR** |
||
|
Cultural feeding practices |
Yes |
61 (85.9) |
10 (14.1) |
3.35 |
3.37 |
|
No |
173 (64.6) |
95 (35.4) |
|||
|
Breastfeeding advice by public health staff during house visit |
Yes |
37 (77.1) |
11 (22.9) |
1.605 |
1.01 |
|
No |
197 (67.7) |
94 (32.3) |
|||
|
Problems during breastfeeding |
Yes |
65 (85.5) |
11 (14.5) |
3.29 |
3.38 |
|
No |
169 (65.43) |
94 (35.7) |
|||
*Crude OR, **Adjusted OR
Discussion
Appropriate breastfeeding practices are necessary to achieve the fourth goal of MDG (Millennium Development Goals), which is reducing child mortality. Kerala is well known for its health indicators comparable with developed countries and its high female literacy rate (15). Despite high educational status and good antenatal care among the study population, breastfeeding practices were not up to the desired level in the study area. Every child should start being breastfed at the earliest. Breastfeeding was initiated within 1 hour of delivery by 2/3rd of the study population. In this study, 223 (65.78%) mothers began breastfeeding within one hour, which was comparable with other studies conducted in India ( 8, 9, 20, 21, 22) and was consistent with the NFHS-5 data of Kerala(16), which was 66.7 %. This percentage was lower, compared to the District Level Household and Facility Survey, in which 78.8% of the mothers initiated breastfeeding within one hour (23). and a study conducted in Africa, in which 72.9% initiated breastfeeding within an hour (24). This was while Patel A et al. (13) in their observed a 23.5%. rate of timely initiation, which was very low. All the children were fed with colostrum in the study area.
The problem of prelacteal feeding was observed in the study population, in line with other studies (7, 12, 25, 26), with the highest proportion belonging to Muslims. This practice is harmful to the newborn as they could introduce infection, sensitizes the gut to foreign proteins, and may delay the onset of lactation (8). The present study showed the prevalence of prelacteal feeding at 7.37%. The prevalence of prelacteal feeding in the present study was very low as compared to other studies conducted in different parts of India, which was from19% (27) to 91.25% (28). This lower prevalence of prelacteal feeding may be due to higher educational status of the mothers in the study population. The most common prelacteal fluid given in the present study was Zam-zam water (holy water from Mecca) among Muslims (52%), followed by lactogen (24%), Honey (12%), water (8%) and cow’s milk (4%). Ghutti and honey were the most common prelacteal feeds in the study by Manish Chadurvedi et al. (7) in New Delhi. According to Vashney A M et al. (12), in Gujarat, animal milk and sugar water were the most common prelacteal fluids.
In the present study, all mothers (100%) have given breast milk to their babies, which was higher than the National Family Health Survey, in which 95.7% of the children in India were ever breastfed and 97.4% in Kerala (9). A study in Uttarakhand by Vyas Shili et al. (29) found the proportion of children ever breastfed to be 93.6%. According to a study in Villages of Karnataka by Banapurmath C R et al., (30) 97% of the children were ever received breast milk.
EBF is recommended because it contains all essential nutrients for the first six months of life. 1/3rd of mothers in the study area did EBF until baby was six months.. Although female literacy rate was higher in Kerala compared with other states, a lower prevalence of EBF was observed in the present study (30.97%), lower as compared to the National level, 46.4% (9), and other studies conducted in different parts of India (26, 29, 31, 32). This percentage was higher than Kerala, which was 22.3% (23). In a population where the mother's educational status is high, and most of them are currently unemployed, EBF can easily be practiced. In addition, this percentage is relevant considering that all the deliveries were institutional and received postnatal feeding advice. In the present study, common reasons for discontinuation of EBF were elders' advice with regard to cultural feeding practices (45.73%), followed by insufficient milk (44.44%) and maternal employment (8.12%). In a study by Nishimura H et al. (33) conducted at rural South India, it found that insufficient milk was the most common factor for early discontinuation of EBF, which was consistent with the findings of the present study. Other studies carried out in India demonstrated that Insufficient milk (42%) and (28.5%), mother's employment (20%), and weight gain of the baby (15%) were the reasons for early discontinuation (8, 34, 22, 29). Diseases like respiratory infections and diarrhoea were significantly higher among infants with EBF for less than six months, similar to other studies (35, 36, 37).
The present study revealed a critical barrier, i.e., elders' advice regarding prevalent cultural feeding practices. Similar findings were observed in a study conducted by Avneet Randhawa et al. (32) at Punjab where it was found that that nuclear families were more likely to exclusively breastfed their babies more than those staying in joint or extended nuclear families. This finding may be due to the cultural practices followed by the elders in the family. Hence, to improve EBF in a state with good health indices and a high literacy rate, focus group discussions may be conducted by involving elders of the house, religious leaders, local leaders, healthcare providers and mothers to address prevailing practices which hamper EBF. EBF is a simple and cost-effective method to reduce common morbidities like acute diarrheal diseases and acute respiratory infections among under-five children. Due to short maternity leave time, the return to work may hamper employed mothers from breastfeeding their infants exclusively for the recommended six months duration. Therefore, adequate support for breastfeeding mothers in the workplace should be ensured.
Since the data collected was pertaining to the previous two years, recall bias may have occurred. As mothers with children of over 2 were included in the study, it is impossible to assess the continuation of breastfeeding for up to 2 years.
Conclusions:
Breastfeeding practices among the women in the study area are not up to the recommended level, even though there is a high level of academic education in the study group. The prevalence of EBF up to 6 months is 30.9%, which is extremely low, compared to the WHO recommendations (100%) and the national average (55.5%) according to NFHS-5 data. This study also highlights certain crucial areas of concern, such as the cultural barriers imposed by the elders in the family, mother's employment, and problems faced by mothers during breastfeeding (insufficient breast milk, cracked nipple, retracted nipple). These factors were statistically consistent with other studies conducted in different parts of India.
Therefore, it is imperative to carry out in-depth studies to identify the gaps in breastfeeding practices and offer tailored interventions such as counselling the mothers and elders in the family antenatally, providing postnatal lactation support and counselling, and considering adequate maternity leave for mothers based on the needs of the study population. This in turn may positively influence breast feeding practices, thereby, improving child health and lowering healthcare costs.
Acknowledgement
The authors would like to thank Dr Sudhiraj T S, Medical Officer In- Charge, from Urban Health Training Centre, Paravattani, Thrissur for his support and cooperation
All the ethical principles have been observed in the present study. The study protocol was approved by the Institutional Research and Ethics Committees of Govt. Medical College, Thrissur
Conflict of interest
Authors declared no conflict of interest.
Funding
This research has not received any funding from any public, private or other organization
Ethical considerations
All the ethical principles have been observed in the present study. The study protocol was approved by the Institutional Research and Ethics Committees of Govt. Medical College, Thrissur
Code of Ethics
Maintained during the entire study period.
Authors’ contributions
All authors contributed to conception, design, and definition of the intellectual content of the study; Data were collected by F. O and J. KS; all authors participated in data analysis, interpretation, and manuscript drafting, and F. O, P. C, S. MV, and R. R provided critical revisions. The final draft of the manuscript was reviewed and approved by all authors.
Open Access Policy
JCHR does not charge readers and their institution for access to its papers. Full text download of all new and archived papers are free of charge.
References
1. World Health Organization. Fact Sheets- Infant and Young child feeding. WHO; 2021. Available at: URL: https://www.who.int/news-room/fact-sheets/detail/infant-and-young-child-feeding. Accessed May 04, 2023.
2. World Health Organization. Indicators for assessing Breast feeding practices. Geneva: WHO; 1991.
3. The World Health Organization. Exclusive breastfeeding for six months best for everywhere. WHO; 2011.
4. Victora CG, Smith PG, Vaughan JP, et al. Evidence for protection against infant deaths from infectious diseases in Brazil Lancet. 1987; 2: 319-22
5. World Health Organization and the United Nations Children’s Fund (UNICEF). Protecting, promoting and supporting breastfeeding in facilities providing maternity and newborn services: implementing the revised Baby-friendly Hospital Initiative; 2018. Available at: URL: http://apps.who.int/iris. Accessed May 04, 2023.
6. Roy MP, Mohan U, Singh SK, et al. Determinants of prelacteal feeding in rural northern India. International journal of preventive medicine. 2014; 5(5): 658.
7. Chaturvedi M, Nandan D, Gupta S. Rapid assessment of infant-feeding practices in Agra district. Indian Journal of Community Medicine. 2007; 32(3): 227.
8. Bhattacharjya H, Das S, Mog C, et al. Breast feeding: Practices and determinants in rural area of west Tripura district of India. National Journal of Community Medicine. 2013; 4(04): 628-31.
9. International institute for population sciences. National Family Health Survey (NFHS-3), 2005-06: India. Vol. I. Mumbai: International Institute for Population Sciences. IIPS O; 2007.
10. Betran AP, De Onis M, Lauer JA, et al. Ecological study of effect of breast feeding on infant mortality in Latin America. Bmj. 2001; 323(7308): 303.
11. World Health Organization. Indicators for assessing infant and young child feeding practices- part 1: Definitions. Conclusions of a consensus meeting held 6-8 November 2007 in Washington D.C. Geneva: WHO; 2008.
12. Varshney AM, Kumar D, Patel M, et al. Determinants Of Breast-Feeding Practices in Urban Slums of a Taluka Headquarter of District Anand, Gujarat. National Journal of Community Medicine. 2012; 3(03): 534-7.
13. Patel A, Badhoniya N, Khadse S, et al. Infant and young child feeding indicators and determinants of poor feeding practices in India: secondary data analysis of National Family Health Survey 2005-06. Food Nutr Bull. 2010; 31(2): 314-33
14. Jones G, Steketee RW, Black RE, et al. How many child deaths can we prevent this year?. The lancet. 2003; 362(9377): 65-71.
15. Office of the Registrar General & Census Commissioner, India 2011. Census of India 2011. India: New Delhi; 2011. Available at: URL: https://censusindia.gov.in/2011- common/censusdataonline.html
16. International institute for population sciences (IIPS) and ICF. National Family Health Survey (NFHS- 5), 2019- 2021: India: Volume 1. Mumbai: IIPS and ICF; 2021.
17. Office of the Registrar General & Census Commissioner, India. Census. India: New Delhi; 2011. Available at: URL: http://www.census2011.co.in/census/state/kerala/html.
18. Kumar BR, Dudala SR, Rao AR. Kuppuswamy’s socio-economic status scale–a revision of economic parameter for 2012. Int J Res Dev Health. 2013; 1(1): 2-4.
19. International Institute for Population Sciences. The Concurrent Evaluation of National Rural Health Mission. Kerala: Mumbai; IIPS; 2009.
20. Dongre AR, Deshmukh PR, Rawool AP, et al. Where and How Breastfeeding Promotion Initiatives Should Focus Its Attention? A Study from Rural Wardha. Indian J Community Med. 2010; 35(2): 226-9
21. Sagar MV, Mane V, Praveenkumar N, et al. A Community Based Study on Infant and Young Child Feeding Practices in Bhadravati Taluk, Shivamogga. Indian Journal of Public Health Research & Development. 2015; 6(3).
22. Satija M, Sharma S, Chaudhary A, et al. Infant and young child feeding practices in a rural area of North India. Asian journal of medical sciences. 2015; 6(6): 60-5.
23. International institute for population sciences. District Level Household and Facility survey (DLHS-4), 2012- 2013. Kerala: Mumbai; IIPS; 2013
24. Dukuzumuremyi JP, Acheampong K, Abesig J, et al. Knowledge, attitude, and practice of exclusive breastfeeding among mothers in East Africa: a systematic review. International breastfeeding journal. 2020; 15: 1-7.https://doi.org/10.1186/s13006-020-00313-9
25. Aarti P, AK R, KA N. Prevalence of exclusive breast feeding and its correlates in an urban slum in Western India. International e-Journal of Science, Medicine and Education. 2009: 14-8.
26. Subbiah N, Jeganathan A. Socio-cultural beliefs influencing breastfeeding practices among primi postnatal mothers residing in urban slum area of Delhi. Health Popul Perspect Issues. 2012; 35(2): 61-73.
27. Madhu K, Chowdary S, Masthi R. Breast feeding practices and newborn care in rural areas: a descriptive cross-sectional study. Indian journal of community medicine: official publication of Indian Association of Preventive & Social Medicine. 2009; 34(3): 243.
28. Yadavannavar MC, Patil SS. Socio cultural factors affecting breast feeding practices and decisions in rural women. International Journal of Plant, Animal and Environmental Sciences. 2011; 1(2): 46-50.
29. Vyas S, Sharma P, Kandpal SD, et al. A community based study on breastfeeding practices in a rural area of Uttarakhand. National Journal of Community Medicine. 2012; 3(02): 283-7.
30. Banapurmath C R, Nagaraj M C, Banapurmath S, et al. Breastfeeding Practices in Villages of Central Karnataka. Indian Pediatr. 1996; 33(6): 477-9.
31. Rahman M, Begum N, Rahman MM, et al. Breast Feeding Practices among Rural Women in a selected area of Bangladesh. Northern International Medical College Journal. 2014; 5(2): 345-8.
32. Randhawa A, Chaudhary N, Gill BS, et al. A population-based cross-sectional study to determine the practices of breastfeeding among the lactating mothers of Patiala city. Journal of family medicine and primary care. 2019; 8(10): 3207.
33. Nishimura H, Krupp K, Gowda S, et al. Determinants of exclusive breastfeeding in rural South India. International breastfeeding journal. 2018; 13(1): 1-7. https://doi.org/10.1186/s13006-018-0178-5.
34. Aldalili AY, El. Mahalli AA. Factors associated with cessation of exclusive breastfeeding. Journal of Multidisciplinary Healthcare. 2021: 239-46. https://doi.org/10.2147/JMDH.S277819.
35. Joseph N, Naik VA, Mahantshetti NS, et al. Factors associated with morbidities among infants in three sub centre areas of belgaum district of south India: A longitudinal study. Indian J Community Med. 2013; 38(3): 168-74.
36. Mihrshahi S, Oddy WH, Peat JK, et al. Association between infant feeding patterns and diarrhoeal and respiratory illness: a cohort study in Chittagong, Bangladesh. International breastfeeding journal. 2008; 3: 1-0.
37. Jennifer HG, Muthukumar K. A cross-sectional descriptive study was to estimate the prevalence of the early initiation of and exclusive breast feeding in the rural health training centre of a medical college in Tamilnadu, South India. Journal of clinical and diagnostic research: JCDR. 2012; 6(9): 1514.
List of abbreviations
|
Abbreviation |
Definition |
|
EBF |
Exclusive breastfeeding up to 6 months |
|
MDG |
Millennium Development Goals |
|
WHO |
World Health Organization |
|
UNICEF |
United Nations Children's Fund |
Received: 2023/04/10 | Accepted: 2023/08/5 | Published: 2024/01/21
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution 4.0 International License. |