Volume 12, Issue 2 (11-2023)
JCHR 2023, 12(2): 236-255 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Azadiyan M, Vosoogh Moghadam A, Farhadimahalli A. What Can We Do to Improve the Health Policy-Making Cycle in the Islamic Republic of Iran with a Good Governance Approach?
Recommendations for the Secretariat of the Supreme Council for Health and Food Security. JCHR 2023; 12 (2) :236-255
URL: http://jhr.ssu.ac.ir/article-1-870-en.html
URL: http://jhr.ssu.ac.ir/article-1-870-en.html
1- Department of Management, Gorgan Branch, Islamic Azad University, Gorgan, Iran
2- 1. Department of Management, Gorgan Branch, Islamic Azad University, Gorgan, Iran 2.Governance and Health Training and Research Group, Neuroscience Research Institute, Tehran University of Medical Sciences and Health Services, Tehran, Iran ,avosooghm@sina.tums.ac.ir
2- 1. Department of Management, Gorgan Branch, Islamic Azad University, Gorgan, Iran 2.Governance and Health Training and Research Group, Neuroscience Research Institute, Tehran University of Medical Sciences and Health Services, Tehran, Iran ,
Full-Text [PDF 698 kb]
(1029 Downloads)
| Abstract (HTML) (1433 Views)
References
1. Mosadeghrad AM, Rahimi-Tabar P. Health system governance in Iran: A comparative study. Razi Journal of Medical Sciences. 2019; 26(9): 10-28. [Persian]
2. Joulaei H, Bagheri-Lankarani K, Zarei N, et al. Stewardship and its role in Iran'shealthsystem: A scoping review. IJHP. 2018; 2: 206-16. [Persian]
3. World Health Organization. Government of South Australia. Adelaide statement on health in all policies. 2010. doi: 10.1093/heapro/daq034.
4. De Leeuw E, Kickbusch I, Palmer N, et al. European Healthy Cities come to terms with health network governance. Health promotion international. 2015; 30(suppl_1): i32-44. doi: 10.1093/heapro/dav040.
5. Alamdari S, Alamdari A. IR Iran national health system strategic architecturing based on national vision 1404: A proposed model. Iranian Journal of Public Policy. 2015; 1(1): 21-42. doi: 10.22059/ppolicy.2015.57150. [Persian]
6. Ebrahimpour H, Eliki F. Investigating the role of good governance in the efficiency of governments. InInternational Conference of Management Elites, Iran; Tehran. 2016; 1. [Persian]
7. Sharifzadeh F, Rahmarallah G. Good governance and the role of government. organizational culture management. 2003; 1(4): 93-109. [Persian]
8. Rahmani K, Rezayatmand R, Sadeghpour N, et al. Policy-making for rationing in the healthcare system: a review to provide suggestions for Iran. Management Strategies in Health System. 2018; 3(3): 249-62. [Persian]
9. Mosadeghrad AM. An integrated health policy making and analysis model. Tehran Univ Med J. 2020; 77(12): 791. [Persian]
10. O’Brien BC, Harris IB, Beckman TJ, et al. Standards for reporting qualitative research: a synthesis of recommendations. Academic medicine. 2014; 89(9): 1245-51.
11. Hong QN, Fàbregues S, Bartlett G, et al. The Mixed Methods Appraisal Tool (MMAT) version 2018 for information professionals and researchers. Education for information. 2018; 34(4): 285-91.
12. Zazerani Y, Reza M. Understanding the Policy Process; an Overview of the Concepts, Theories, and Models of Policy Process. Iranian Journal of Public Policy. 2018; 3(4): 189-202. [Persian]
13. Shankardass K, Muntaner C, Kokkinen L, et al. The implementation of Health in All Policies initiatives: a systems framework for government action. Health research policy and systems. 2018; 16(1): 1-0. doi: https://doi.org/10.1186/s12961-018-0295-z
14. Strehlenert H, Richter-Sundberg L, Nyström ME, et al. Evidence-informed policy formulation and implementation: a comparative case study of two national policies for improving health and social care in Sweden. Implementation Science. 2015; 10: 1-0. doi: 10.1186/s13012-015-0359-1.
15. Babaei S, Tavakoli G. A policy making process model for public organizations. Public Policy 2015; 1(3): 29-53. doi: 10.22059/ppolicy.2015.57678. [Persian]
16. Maher A, Maziar P. Health policy making process: a systematic review article, Shahid Beheshti University of Medical Sciences, Tehran, Iran. [Persian]
17. Azline A, Iszaid I, Syahira S, et al. Policy arena of health policy-making process in developing countries. International Journal of Public Health and Clinical Sciences 2018; 5(3): 32-48.
18. Ministry of Social Affairs and Health of Finland, in collaboration with the National Institute for Health and Welfare of Finland (THL), the European Observatory on Health Systems and Policies, and the United Nations Research Institute for Social Development (UNRISD). Health in all policies: seizing opportunities, implementing policies; Finland. 2013; 25-287.
19. Zuckerman AM. Successful strategic planning for a reformed delivery system. Journal of Healthcare Management. 2014; 59(3): 168-72.
20. Kokkinen L, Muntaner C, O’Campo P, et al. Implementation of Health 2015 public health program in Finland: a welfare state in transition. Health Promotion International. 2019; 34(2): 258-68.
21. Uneke CJ, Ezeoha AE, Ndukwe CD, et al. Research priority setting for health policy and health systems strengthening in Nigeria: the policymakers and stakeholders perspective and involvement. Pan African Medical Journal. 2014; 16(1).
doi:10.11604/pamj.2013.16.10.2318.
22. Damari BA, Monazzam K, Salarianzadeh H. Where and how to make wise policies for health? A qualitative study on the characteristics of health policy system in the Islamic Republic of Iran. Hakim Journal. 2011; 13(4): 210-8. [Persian]
23. Nasrollapour-Shirvani SD, Motlagh ME, Shariati M, et al. The Strategic Plan of Iranian Medical Sciences Universities: From Theory to Practice. Health Information Management. 2016; 12(6): 770-6. [Persian]
24. Alam AY, Alabdulaali MK. Hospital vision and mission strategic planning and departmental performance. J Pak Med Assoc. 2015; 65: 345-46.
25. Bowen G, Bowen D. Strategy formulation and uncertainty in environments. Journal of Business and Economics. 2014; 5(12): 2315-26. doi: 10.15341/jbe(2155-7950)/12.05.2014/012.
26. Gholipor R, Mafimoradi S, Rahnavard F, et al. Systematic Analysis of Research Articles on Health Policy in the Developing Countries: Implications for Researchers. Journal of Iranian Public Administration Studies. 2019; 2(2): 25-45. doi: 10.22034/jipas.2019.91495. [Persian]
27. Hyder AA, Corluka A, Winch PJ, et al. National policy-makers speak out: are researchers giving them what they need?. Health policy and planning. 2011; 26(1): 73-82. doi: 10.1093/heapol/czq020.
28. Mafimoradi S, Gholipour R, Rahnavard F, et al. How Health Policies change in Islamic Republic of Iran? A substantive theory to understand the policy process. Payesh (Health Monitor). 2020; 19(6): 673-91. doi: 10.29252/payesh.19.6.673. [Persian]
29. Mosadeghrad AM, Rahimi-Tabar P. Health system governance in Iran: A comparative study. Razi Journal of Medical Sciences. 2019; 26(9): 10-28. [Persian]
30. World Health Organization. Everybody’s business: strengthening health systems to improve health outcomes: WHO’s framework for action. Production. 2007: 1-56.
31. Davies C. Links between Governance, Incentives and Outcomes: A Review of the Literature National Co-ordinating Centre for NHS Service Delivery and Organisation R&D. London: The Stationery Office. 2005.
32. World Health Organization. Governance for Health in the 21st Century. WHO Europe; 2012.
33. Lankarani KB, Alavian SM, Peymani P. Health in the Islamic Republic of Iran, challenges and progresses. Medical journal of the Islamic Republic of Iran. 2013; 27(1): 42.
34. Moghadam AV,Damari B, Alikhani S, et al. Health in the 5 th 5-years development plan of Iran: main challenges,general policies and strategies. Iran J Public Health. 2013; 42(1): 42–49. [Persian]
35. Jafari F, HajiNabi K, Jahangiri K, et al. Good governance in the health system: A qualitative study. International Transaction Journal of Engineering, Management, & Applied Sciences & Technologies. 2019; 8: 1127-41. [Persian]
36. Saltman RB, Duran A. Governance, government, and the search for new provider models. International journal of health policy and management. 2016; 5(1): 33.
37. Emami M, Shakeri H. Good governance and The constitution of the Islamic Republic of Iran. Journal of Comparative Law. 2015; 1(2): 25-57. [Persian]
38. Alvaani SM, Alizadeh Saani M. Analyzing the Quality of Good Governance in Iran. Management Studies in Development and Evolution. 2007; 18(53): 1-24. [Persian]
39. Taqvaei AA, Tajdar R. An introduction to good urban governance in an analytical approach. Urban Management. 2009; 23(1): 45-58.
40. Maesoumi Z, Sanei M, Hematian H. A model for effective implementation of health policy in Iran. Quarterly Journal of Management Strategies in Health System. 2019; 4(2): 125-35. [Persian]
41. Afrasiabi, M. Indicators of good governance in the health system [M.Sc. thesis]. Iran. Islamic Azad University Safadasht; 2017. [Persian]
42. Pinterič U. Rethinking public policies Faculty of Organization Studies: Slovenia, Nova Mesto. 2014: 7-75.
43. Houngbo PT, Coleman HL, Zweekhorst M, et al. A model for good governance of healthcare technology management in the public sector: learning from evidence-informed policy development and implementation in Benin. PloS one. 2017; 12(1): e0168842.
44. Valera Mt, Hartigan-Go Ky, Visperas Mk. A Framework to Promote Good Governance in Healthcare.
45. Tabrizi JS, Pourasghar F, Nikjoo RG. Governance of iranian primary Health Care System: perceptions of experts. Iranian Journal of Public Health. 2019; 48(3): 541. [Persian]
46. El-Jardali F, Lavis JN, Ataya N, et al. Use of health systems evidence by policymakers in eastern Mediterranean countries: views, practices, and contextual influences. BMC health services research. 2012; 12(1): 1-20.
47. Jönsson K, Phoummalaysith B, Wahlström R, et al. Health policy evolution in Lao People’s Democratic Republic: context, processes and agency. Health policy and planning. 2015; 30(4): 518-27.
48. Khankeh HR, Lankarani KB, Zarei N, et al. Three decades of healthcare system reform in Iran from the perspective of universal health coverage: A macro-qualitative study. Iranian Journal of Medical Sciences. 2021; 46(3): 198. [Persian]
49. Malek Mohammadi HR, Vahdaninia V. The evolution of health policy: Transition to the governance paradigm for health. Iranian Journal of Public Policy. 2016; 2(2): 73-94. [Persian]
50. Vahdaninia V, Vosoogh Moghaddam A. Understanding late logic of health policy making: The transition to governance for health. Payesh (Health Monitor). 2018; 17(6): 631-46. [Persian]
51. Greer S, Wismar M, Figueras J. EBOOK: strengthening health system governance: better policies, stronger performance. McGraw-Hill Education (UK); 2015.
52. Cabral-Bejarano MS, Nigenda G, Arredondo A, et al. Stewardship and governance: structuring dimensions for implementation primary health care policies in Paraguay, 2008-2017. Ciência & Saúde Coletiva. 2018; 23: 2229-38.
53. Escobar-Ballesta M, García-Ramírez M, De Freitas C. Taking stock of Roma health policies in Spain: lessons for health governance. Health Policy. 2018; 122(4): 444-51.
54. Atun R. Transforming Turkey's health system—lessons for universal coverage. New England Journal of Medicine. 2015; 373(14): 1285-9.
55. Nicholson C, Hepworth J, Burridge L, et al. Translating the elements of health governance for integrated care from theory to practice: a case study approach. International Journal of Integrated Care. 2018; 18(1).
56. Liu SX, de Bont C. Barriers to strategic design: A perspective from China. She Ji: The Journal of Design, Economics, and Innovation. 2017; 3(2): 133-45.
57. Purehtesham M. Studying the effect of governance quality on health indicators in the countries of South-Western Asia. Social Welfare Quarterly. 2018; 18(69): 184-59.
Full-Text: (430 Views)
| What Can We Do to Improve the Health Policy-Making Cycle in the Islamic Republic of Iran with a Good Governance Approach? Recommendations for the Secretariat of the Supreme Council for Health and Food Security |
Marziyeh Azadiyan 1  , Abbas Vosoogh Moghaddam 2 *
, Abbas Vosoogh Moghaddam 2 *  , Ali Farhadi Mahalli 3
, Ali Farhadi Mahalli 3 
 , Abbas Vosoogh Moghaddam 2 *
, Abbas Vosoogh Moghaddam 2 *  , Ali Farhadi Mahalli 3
, Ali Farhadi Mahalli 3 
- Department of Management, Gorgan Branch, Islamic Azad University, Gorgan, Iran
- Department of Management, Gorgan Branch, Islamic Azad University, Gorgan, Iran- Governance and Health Training and Research Group, National Institute of Health Research, Tehran University of Medical Sciences and Health Services, Tehran, Iran
- Department of Management, Gorgan Branch, Islamic Azad University, Gorgan, Iran
| ARTICLE INFO | ABSTRACT | |
| Review Received: 09 Feb 2023 Accepted: 16 May 2023 |
Background: The primary purpose of the health system is to promote equitable health in society. The aim of this study is to offer some recommendations for improving the Iranian health policy-making cycle with a good governance approach. Methods: The systematic review approach was employed to undertake this research. To track down articles published electronically between 2010 and 2021, a comprehensive search in the National Library's English databases, in December 2021, was conducted using the keywords such as public policy, policy, policy-making, health policy, good governance, health, and healthcare. In addition, the Persian equivalents of the aforementioned keywords were searched separately or in combination with Boolean operators (OR, AND) in databases such as Scopus, Ovid, Science Direct, Web of Knowledge, PubMed, IranMedex, Magiran, and SID to further pinpoint the desired articles. To evaluate and validate the quality of the selected articles, critical tools appropriate for the type of study were utilized (e.g., the SRQR tool for qualitative studies and the MMAT tool for mixed-methods studies), and finally, the research team conducted content analysis and categorized the findings. Results: Findings revealed that the health policy-making cycle is an extensive and intra-sectoral concern. Good governance in the health system results in specialized and individualized opportunities for better health and reduces inequality. To accomplish this purpose, it is necessary to emphasize cross-sectoral participation, social responsiveness, and transparent processes, and incorporate the viewpoints of experts and implementers of the health policy-making system. Furthermore, the health system's sovereignty and progress toward good governance should be evaluated, which results in effective policies and health justice. Conclusion: Considering the legal mission of the Supreme Council of Health and Food Security (the highest policy-making authority in the Ministry of Health), it is recommended that the council implement the practical recommendations of this research in actualizing and incorporating the good governance approach into the health policy-making cycle. Keywords: Policy-Making, Learning Health System, Iran |
|
 |
||
Corresponding Author: Abbas Vosoogh Moghaddam avosooghm@sina.tums.ac.ir |
How to cite this paper:
Azadiyan M, Vosoogh Moghaddam A, Farhadi Mahalli A. What Can We Do to Improve the Health Policy-Making Cycle in the Islamic Republic of Iran with a Good Governance Approach? Recommendations for the Secretariat of the Supreme Council for Health and Food Security. J Community Health Research 2023; 12(2): 236-255.
Introduction
Azadiyan M, Vosoogh Moghaddam A, Farhadi Mahalli A. What Can We Do to Improve the Health Policy-Making Cycle in the Islamic Republic of Iran with a Good Governance Approach? Recommendations for the Secretariat of the Supreme Council for Health and Food Security. J Community Health Research 2023; 12(2): 236-255.
Introduction
The health system encompasses all organizations, institutions, groups, and individuals in public and private domains involved in policy-making, resource generation, and financing health interventions with the purpose of reestablishing, promoting and sustaining people’s health (1). The World Health Organization's (WHO) three main goals for health systems are as follows: 1) Improving people's health in society; 2) Ensuring that people's participation in financing the health system is equitable; 3) Meeting people's non-medical expectations, illustrating the value of respect, authority, and confidentiality. To accomplish these objectives, any health system must coordinate 6 functions, namely, governance and leadership, financing, service provision, human resources, information, pharmaceutical and health products (2). In the stewardship approach, the tool of "health policy" refers to the actions undertaken to accomplish specified health service goals in a community (3). The significant contribution of health system policy in promoting health, minimizing health inequities, and fostering economic development is becoming more universally acknowledged (4). It should be highlighted that governance is a compilation of government-created rules and regulations which must be followed by government agents. Furthermore, seven components of health system governance comprise the organizational structure, inter-sectoral communication and cooperation, legislation, policy-making and planning, stewardship, monitoring and evaluation, and customer protection (5). More specifically, high-quality governance in health policy-making plays a very crucial role in determining the health system's progress. With the intention of supplying health care at the foreground of all countries' agendas, the establishment of effective policy-making procedures within the health system is an imperative and significant concern (7). The eight components of good governance are participation, agreement, responsiveness, transparency, accountability, effectiveness, inclusiveness and equity, and the rule of law (9). The Supreme Council of Health and Food Security is an inter-sectoral council chaired by the president and secretary of the Minister of Health. It includes six ministers: Minister of Home Affairs; Minister of Industry, Mine and Trade; Minister of Cooperatives, Labor and Social Welfare; Minister of Education; Minister of Agriculture Jihad; Minister of Sport and Youth, and leaders of organizations including Broadcasting Organization; Plan and Budget Organization; Imam Khomeini Relief Foundation; Institute of Standards and Industrial Research of Iran, along with one member of each of the commissions of health, social, planning and budget and the Islamic Consultative Assembly which acted as an observer. The Islamic Consultative Assembly is responsible for promoting health and food security, reviewing and enacting programs and sectoral and intra-sectoral measures to implement health policies, enact health-oriented national standards for major development plans and regulatory mechanisms, and review regulatory reports, as well as other health related policy-making concerns. In addition, in recent decades, numerous administrators and researchers in the health system have taken significant initiatives to propose reforms to the policy-making process and reconsider the structures in order to attain a more rational and reasonable framework for health system policy-making. However, there are still numerous hidden directions and high-priority issues which may be offered; they are in urgent need of health system policy-making and reforms in various sections. This is only practical with an effective health system governance framework in place. While examining the health policy-making cycle, this study explores the concept and indicators of good governance in relation to health system policy-making and makes some recommendations for improving the Iranian health policy-making cycle with a good governance approach.
Methods
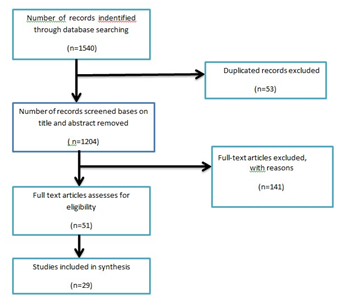
The current study adopted a systematic review approach. To track down articles published electronically between 2010 and 2021, a comprehensive search in the National Library's English databases was carried out using the keywords (the research team came up with the keywords through brainstorming, and then, confirmed them using mesh) such as public policy, policy, policy-making, health policy, good governance, health, and healthcare. Moreover, Iranian Digital Medicine, Science Direct, Ovid, Scopus, PubMed, Web of Knowledge, and Web of Science were searched. The Scientific Information Database (SID) and the database of Iranian journals (Magiran) (IranMedex) were also examined for Persian language papers published between 2010 and 2021 on the keywords such as governance, government, governor, good governance, policy, policy-making, and health policy-making. The process of searching was performed separately or in combination with Boolean operators (OR, AND) in December 2021.A random check of the search process's reliability was undertaken by one of the researchers to ensure that no study was eliminated. Ultimately, the articles that were relevant were carefully selected. Following the selection of relevant studies, important tools suited for the purpose of study were employed to evaluate the quality of the articles. For qualitative studies, the SRQR tool (10) and for mixed-methods studies, the MMAT tool (11) were used. Along with evaluating the quality of publications, other inclusion criteria were: investigations performed between 2010 and 2020, inquiries done in Persian and English, and articles published in highly prestigious and scientific journals. Exclusion criteria were articles whose full text could not be retrieved, theoretical studies, news, letters, policies, and the research undertaken outside the health system. Subsequently, content analysis of the articles was operated (both using the framework and manually), and policy recommendations were established based on the extracted findings in order to improve the Iranian health policy-making cycle with a good governance approach. It must be pointed out that this research regarded minimizing information distortion, avoiding conflicts of interest, informing relevant organizations about the outcomes of the research, and intellectual property rights as ethical considerations. This article is derived from a PhD dissertation on public management (a subfield of public policy-making) authorized by the Islamic Azad University of Gorgan (Iran country) on 2021/7/18 under the code 162280383.
Results
Through searching the keywords, 1540 articles were retrieved. When these articles were reviewed in light of the inclusion criteria specified in the methods section, 29 cases were selected. 10 articles were published in Persian, while the remaining 19 were in English. 13 papers focused on the health policy-making cycle, 10 on governance (health system governance(, (Chart 1, Table 1, Table 2).
Methods
The current study adopted a systematic review approach. To track down articles published electronically between 2010 and 2021, a comprehensive search in the National Library's English databases was carried out using the keywords (the research team came up with the keywords through brainstorming, and then, confirmed them using mesh) such as public policy, policy, policy-making, health policy, good governance, health, and healthcare. Moreover, Iranian Digital Medicine, Science Direct, Ovid, Scopus, PubMed, Web of Knowledge, and Web of Science were searched. The Scientific Information Database (SID) and the database of Iranian journals (Magiran) (IranMedex) were also examined for Persian language papers published between 2010 and 2021 on the keywords such as governance, government, governor, good governance, policy, policy-making, and health policy-making. The process of searching was performed separately or in combination with Boolean operators (OR, AND) in December 2021.A random check of the search process's reliability was undertaken by one of the researchers to ensure that no study was eliminated. Ultimately, the articles that were relevant were carefully selected. Following the selection of relevant studies, important tools suited for the purpose of study were employed to evaluate the quality of the articles. For qualitative studies, the SRQR tool (10) and for mixed-methods studies, the MMAT tool (11) were used. Along with evaluating the quality of publications, other inclusion criteria were: investigations performed between 2010 and 2020, inquiries done in Persian and English, and articles published in highly prestigious and scientific journals. Exclusion criteria were articles whose full text could not be retrieved, theoretical studies, news, letters, policies, and the research undertaken outside the health system. Subsequently, content analysis of the articles was operated (both using the framework and manually), and policy recommendations were established based on the extracted findings in order to improve the Iranian health policy-making cycle with a good governance approach. It must be pointed out that this research regarded minimizing information distortion, avoiding conflicts of interest, informing relevant organizations about the outcomes of the research, and intellectual property rights as ethical considerations. This article is derived from a PhD dissertation on public management (a subfield of public policy-making) authorized by the Islamic Azad University of Gorgan (Iran country) on 2021/7/18 under the code 162280383.
Results
Through searching the keywords, 1540 articles were retrieved. When these articles were reviewed in light of the inclusion criteria specified in the methods section, 29 cases were selected. 10 articles were published in Persian, while the remaining 19 were in English. 13 papers focused on the health policy-making cycle, 10 on governance (health system governance(, (Chart 1, Table 1, Table 2).
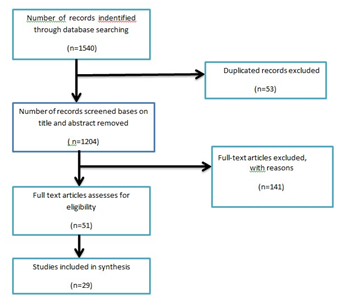
Figure 1. Flow diagram of the search, selection and screening of the studies
Table 1. Characteristics of the studies included in the systematic review
| No | First author | Year | Title | Country | Type of study | The purpose of the study | Major findings |
| 1 | Hydar Adnan | 2010 | National policymakers speak out: Are researchers giving them what they need? | Egypt | Qualitative | Providing some obstacles to the process of policy-making | According to the findings of interviews with policymakers in Iran, Argentina, Egypt, Malawi, Oman, and Singapore, the barriers to the use of evidence and research in the policy process include the following: the policymakers' lack of knowledge about research techniques, their inability to use them, and the influence of the political context, lack of technical capacity to use research findings; lack of use of social networks; and a structured entity for research in the Ministry of Health. |
| 2 | Damari | 2011 | Where and how to make wise policies for health (a qualitative study on the characteristics of health policy system in the Islamic Republic of Iran) | Iran | Qualitative | Offering the characteristics and prerequisites of the health policy system | Features of a reasonable health policy-making system included stakeholders' participation, social accountability, , securing implementation, meritocracy, job security, being evidence-based, and having the ability for coordination and collaboration. |
| 3 | Shukla | 2013 | How to govern the health sector and its institutions effectively | America | Qualitative | Delivering solutions for health system governance | Effective health system management necessitates that decisions be made on the basis of the information, evidence, and shared values, entailing an inclusive, transparent, and responsive process regarding the demands of the individuals served by the ministry or organization. Those who render and enact decisions are to be held accountable; strategic goals should be addressed effectively, efficiently, ethically, and equitably; and the good governance would improve the vitality of the ministry or organization. |
| 4 | Uneke | 2013 | Research priority setting for strengthening health policy and health systems in Nigeria: The policymakers and stakeholders perspective and involvement |
Nigeria | Qualitative | Determining effective factors for health policy prioritization and strengthening health systems in Nigeria | Increasing the group of competent and trained experts involved in policy-making is extremely important and effective, as is considering an adequate budget, having up-to-date, complete, accurate, valid, useful and comparable information , ,and incorporating the viewpoints of researchers and other experts and stakeholders in decision-making , policy-making ,and prioritization |
| 5 | Jakubowski | 2013 | Changing the national role in health system governance: A case study on Australia and 11 European countries | Norway | Qualitative | Examining health governance in 11countries to improve health policy and implementation | The findings of 11 European countries and Australia's policy evaluations demonstrated that policy priorities and the process by which health decisions are determined are crucially important for health policy reform, regulation, and management. |
| 6 | Leppo | 2013 | The health sector’s role in Health in All Policies (HiAP) | England | Qualitative | Bringing up necessary components to adopt the HiAP viewpoint | Addressing the concern regarding the requirements to implement the HiAP perspective |
| 7 | Hartingan | 2013 | A framework to promote good governance in healthcare system | Ireland | Qualitative | Providing a framework for good health system governance | Health reform and anti-corruption strategies necessitate a governance model. The government must successfully execute efficient policies for good governance in the health system. |
| 8 | Strehlenert | 2015 | Evidence–informed policy formulation and implementation: A comparative case study of two national policies for improving health and social care in Sweden | Sweden | Qualitative | Providing a conceptual model for policy-making process |
Proposing the conceptual model of evidence –informed policy formulation and implementation |
| 9 | Babaiee | 2015 | Developing a model for the policy process in government organizations | Iran | Qualitative |
Providing a model for policy- making process in government organizations
|
The author introduces a model which consists of four major stages: problem-solving, policy formulation, policy implementation, and subsequent evaluation, with detailed descriptions of the procedures involved in each stage and their relationships. |
| 10 | Greer | 2016 | Strengthening the health system governance: Better policies and stronger performance | England | Qualitative | Providing factors which improve the health policy- making process | The article discussed and reviewed health policies in Australia, Belgium, Finland, Ireland, Norway, Slovenia, Sweden, and the United Kingdom. It concluded that it is of paramount importance to pay attention to law and policy-making with the cooperation of all stakeholders and other responsible organizations outside the system, as well as establishing macro and quantitative goals and strategies for policy reinforcing. |
| 11 | Malek Mohammadi | 2016 | The evolution of health policy: Transition to the governance paradigm for health | Iran | Qualitative | Providing necessary items for health policy-making and governance | Intersectoral actions, healthy public policy, and health in all policies are the three major policy trends that, along with a transformation in political paradigms, have resulted in the emergence of a new viewpoint on health governance. |
| 12 | Saltman | 2016 | Governance, government, and the search for new provider models | Belgium | Qualitative | Examining the health system's governance and exploring new governance models for the health system | The transformation of health governance to execute policies consistent with good governance must reflect the practical operational realities in order to have the intended effect on health sector's reform outcome. |
| 13 | Chanturidze | 2016 | Governance of health requires evidence and the exchange of information | Argentina | Qualitative | Examining governance and supplying resources for an applicable framework for policies, as well as improving performance in the execution of health system policy |
The notion of governance must be properly described and operationalized in order to be useful for policy debate and for the development of an appropriate framework for performance improvement. |
| 14 | Houngbo | 2017 | Designing a model for good governance in technology management of the public health system in Benin | Benin | Qualitative | Developing a model for good governance in the technology management of Benin's public health system | The role of actors in policy implementation is indispensable, and supporting individuals who control corruption and consider ethical considerations as principles of good governance in the health system was discussed. |
| 15 | Piouneh | 2017 | A framework for assessing the sovereignty of the health system | Australia | Qualitative |
Providing a framework for evaluating health system governance
|
In order to successfully implement health system policies, countries must assess the sovereignty of the health system and work toward good governance in order to improve the sovereignty of the health system. |
| 16 | Nicholson | 2018 | Translating the elements of health governance for integrated care from theory to practice: A case study approach | Sweden | Qualitative | Examining health governance and implementation barriers for health system policies to improve health governance | The three primary impediments to applying health system policies are management, interaction with other organizations, and a high degree of concentration in the application of inter-organizational policies, which necessitates a change in health system governance. |
| 17 | Afrasiabi | 2018 | Indicators of good governance in the health system | Iran | Qualitative | Components of good governance in the health system | By examining good governance principles in general, it articulated the principles of partnership between the sector and stakeholders, accountability and interaction between people and policy implementers, transparency in policy and practice, corruption control, and ethics as principles of good governance in the health system. |
| 18 | Pourehtesham | 2018 | Studying the effect of governance quality on health indicators in the countries of south-western Asia | Iran | Qualitative | Investigating the relationship between governance quality and health in Southwest Asian countries | The six indicators of governance have a significant influence on health outcomes and may also help reduce mortality, hence increasing life expectancy at birth and improving health system indicators. |
| 19 | Jafari | 2018 | Explaining the indicators of good governance in the health system | Iran | Qualitative | Examining the components and requirements of good governance in Iran's health system | Countries must identify their national and internal models of good governance and use their history, culture, and specified values to accomplish this purpose. Interaction between departments and collaboration with other government organizations, among other things, is beneficial for health system governance. |
| 20 | Azline | 2018 | Policy arena of health policy-making process in developing countries | Slovenia | Qualitative | Examining health policy in developing nations and determining successful factors for health policy making |
Economic, social, and political structures all have an impact on health policy-making and the description of the activities that should be undertaken in bureaucratic, administrative, and legislative sectors. |
| 21 | Yazdani | 2018 | Understanding the policy process: An overview of the concepts, theories, and models of policy process | Iran | Qualitative | The recognition of the public policy- making, a general look at concepts, theories and models | This article will familiarize readers with a variety of topics, including the definition of public policy, the process by which public policies are developed, the types of models that can be used to create/evaluate public policy, and a summary of how public policy-making appears to fit into the American government process. |
| 22 | Maesoumi | 2019 | A model for effective implementation of health policy in Iran | Iran | Qualitative | Offering the essential factors for the implementation model of Iran's health system policies | Improved quality of the policies' implementation fosters mutual trust between the Iranian health system and various levels of the target community, enhances motivation, reinforces the essence of cooperation, facilitates teamwork among executives, creates an optimal environment for creativity and innovation in policy implementation, empowers health indicators in the community, and obtains credibility for the health system in Iran. |
| 23 | Vahdaninia | 2019 | Understanding late logic of health policy-making: The transition to governance for health | Iran | Qualitative | Examining the health system's governance and the required criteria for successful health system governance | Governance for health is not exclusively an action, but a 'value system' and a 'sociocultural perception' of 'sustainable development' which may result in an equitable opportunity for better health and a decrease in inequalities. Additionally, a communicative focus on intersectoral collaboration and multi-sectoral coordination for health strengthens the systemic characteristics of public policy and may result in more successful programs across all policy domains. |
| 24 | Mosadeghrad | 2019 | Health system governance in Iran: A comparative study | Iran | Qualitative | Providing solutions for the effective governance of Iran's health system | To promote health system governance, it is recommended that an integrated health system model be developed to incorporate health system enablers (building blocks) and outcomes; so that the number of directors in the Ministry of Health will be reduced, communication with other external organizations can be established, resulting in policy-making and planning. Furthermore, leadership, management and stewardship can be enhanced, and a comprehensive standard for evaluation of healthcare organizations will be developed. |
| 25 | Gholipor | 2019 | Systematic analysis of research articles on health policy in the developing countries: Implications for researchers | Iran | Qualitative | Analysis and systematic review of the health policy research in developing countries, including recommendations for researchers in this field | Efforts made in developing countries to elucidate changes in the process of health policy formulation have been restricted. Therefore, additional qualitative investigations employing rigorous research methodologies are required to further improve existing theories or generate new ones with the goal of improving knowledge of the health policy process in developing countries. |
| 26 | Tabrizi | 2019 | Governance of Iranian primary health care system: Perceptions of experts |
Iran | Qualitative | Presenting the key elements of primary health care governance in Iran's health system | The components identified as essential pillars and components for the Iranian PHC (Primary health care) governance model included quality improvement, management and leadership, community involvement and customer participation, the effectiveness of PHC, human resource development, safety, health care evaluation, and health information management. |
| 27 | Mafimoradi | 2020 | How health policies change in Islamic Republic of Iran?: A substantive theory to understand the policy process | Iran | Qualitative | Examining ways to change the country's health policy system and proposing a conceptual model in this respect | The primary driver of change in health policies is 'impression- making,' for which its proprietors engage in three contextual domains of agenda-setting, documentation, and implementation, employing certain strategic patterns to accomplish the goal. Impression, as the primary determining stream in the health domain, necessitates matching four underlying streams of politics, idea, vertical individualism, and in order to conceptualize its owners' intended impressions. As long as impressions are formed, change is in progress. By diverging from any contextual streams or lowering the desire to create an impression, the change is stopped or degraded irrespective of the problem to be addressed or the policy to be implemented properly. |
| 28 | Maher | 2020 | Health policy-making process: A systematic review article | Iran | Qualitative | Examining the policy-making process in Iran's health system and identifying successful elements for policy-making in this domain | The process of health policy-making is extensive and cross-sectoral, and at each level, the assistance of government organizations, private organizations, specialists, researchers, and international organizations, as well as experiences learned from other countries, must be utilized. |
| 29 | Mosadeghrad | 2020 | A practical model for health policy-making and analysis | Iran | Qualitative | Using the principles of strategic management and an analysis of Iran's health policies, the features of an integrated health policy model is presented. | Using the principles of strategic quality management, an integrated model of health policy-making and analysis was developed for the Iranian health system. This model is comprised of five distinct phases and ten different steps. 1. Forming incentives, which includes the formulation of a problem statement and the establishment of political agreements. 2. The policy preparation phase, which entails the construction of a policy secretariat, the analysis of stakeholders in order to form a strong coalition, and lastly, the solicitation of support to improve policy. 3- Policy formulation involves agenda-setting, policy content formulation, and policy legislation. 4- Policy implementation includes the acceptance, adaptation, and implementation of policies. 5. Policy evaluation comprises evaluating policy constituents, outcomes, and the policy-making process. |
Table 2. Number of articles based on the year of publication
| 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | 2019 | 2020 | Year |
| 1 | 1 | 0 | 5 | 0 | 2 | 4 | 2 | 6 | 5 | 3 | Number |
| 3/45 | 3/45 | 0 | 17/2 | 0 | 6/89 | 13/76 | 6/89 | 20/84 | 17/2 | 10/32 | Percentage |
The following conclusions are drawn from the present study's analysis and review of papers which were summarized and classified.
Health policy-making
Identifying issues and developing evidence-based models of problems, bringing other organizations together according to their responsibilities, looking for support to solve problems, soliciting new ideas and mediating and negotiating to achieve a policy plan, prioritizing policy design, and managing the policy process are among the Ministry of Health's most important responsibilities. These responsibilities are consistent with the policy-making process (12). Management of the health system will take place across all sectors and levels, despite their structural differences (13). The decisions made must be enforceable, frequently monitored, and modified if necessary. Moreover, the Ministry of Health must be capable of mobilizing resources and resolving problems via the engagement of all stakeholders and government agencies associated with health, as well as integrating the experience and recommendations from professionals in this field (12). The policy-making process is discussed in detail in the majority of the extracted articles as problem identification, policy formulation, policy implementation, and performance evaluation (14). This process is the same in the majority of countries. Policymakers in government organizations can use an analytical system and expert committees to address the policy-making process by removing human and organizational constraints and implementing a comprehensive model (13). Several critical points should be taken into consideration, which include determining the root cause of the problem, formulating a policy based on previous evaluations, maintenance, performance monitoring, evaluating the process in which the problem occurs, and final evaluation (15). The role of policymakers is extremely important, as is their capacity to understand the organization's values, unify those involved in this sector, and utilize all the aspects involved in policy-making (16). Policymakers play a more important role in the health system than other organizations (17). Policy formulation and implementation occurs following the collection of evidence and consultation with stakeholders (18). Prioritization is an extremely crucial element (19). Focusing on health prioritization is important due to the lack of resources and the need for appropriate resource allocation, the complexity, and dispersion of health care providers, and uncertainty and rapid change. It is worth noting that adaptability occurs more readily when managers and leaders have a clear orientation, strategy, and coordination in this regard (20). In the spirit of the complications and significance of health policy-making, planning for policy implementation is of paramount significance (16). Globalization and decentralization, the involvement of social media, and pressure groups in the policy-making process are important (18). International support is another aspect in policy-making (20). The political and social structure of countries has a major effect in policy-making (17). The influence of political communication and the form of government on policy-making demonstrates the prevalence of health in all policies (20). In addition, using research and evidence in policy marking is vital (21). Policy formulation depends on its type; hence, one framework or model cannot always be utilized for all kinds of policies (14). Political, economic, and social structures also play a role in policy-making; although, the success of policy-making rests solely on what occurs in practice (e.g., practical considerations) (22). Through workshops and national education programs, the importance of managers participating in the formulation process and considering high-level policy documents should be emphasized for optimal policy-making (23). Successful organizations are those that can implement what they formulate (24). It is recommended that stakeholders receive feedback on implementation issues (25). A large body of research has revealed a variety of operational barriers. The following factors have been identified as contributing to policy-making failures in the majority of investigations.; the complexities and lack of transparency surrounding policies and programs, the time and energy spent formulating them, the inaccuracy with which constraints and obstacles are identified, the lack of recognition and transparency surrounding departmental responsibilities and communication with organizations outside of health agencies and collaboration in this area, Stakeholders' uninvolvement in the formulation process, which frequently results in implementation gaps, the lack of appropriate financial resources, and the focus of the majority of ministries on operations in specific communities such as hospital services or on illnesses and conflicts in daily crisis management (26). The main motives for health policy failure or success are incomprehension of the policy formulation process, identification of the impact and the role of each of the players involved, and ultimately an attempt to balance these factors, particularly in relation to the power of several key players. It is in such a way that the failure of some policies to achieve their objectives can be attributed to disregarding some of the factors influencing the analysis stage (26). Other factors contributing to the failure of some programs include policymakers' lack of knowledge about research procedures and their inability to employ research in health policy-making (27). The majority of studies recommended the proliferation of a model for the health system's policy-making process, which would encompass the preliminaries steps for the formulation, implementation, evaluation, and sustainability of policy products. Several studies addressed the evolution of health system governance and the move toward a more contemporary perception of good governance.
Health system governance
Sovereignty or governance refers to a collection of government-imposed laws and regulations which must be enforced by government agents (28, 29). The purpose of governance is to design an appropriate structure for achieving organizational goals, select and appoint individuals within the organizations, formulate policies and regulations, determine the organization's strategic direction, manage resources necessary to implement policies, ensure the implementation of high-level rules, and supervise, monitor and control the organization's performance (30, 31). Developing countries confront challenges in health system governance. Many of these challenges lack knowledge and skills in health policy formulation and management, participation of all stakeholders in health policy formulation, and might fail to pay attention to all factors affecting health. They may also lack an incoherent approach to the health formulation process, have an ineffective leadership regarding health reform, and not implement all rules and regulations and periodically evaluate them (32). Iran's health system governance is also confounded by challenges, including the overlapping health system and other executive organizations responsibilities, unsatisfactory implementation of the structure approved by the Ministry of Health, lack of transparency regarding individual responsibilities, authority, and responsiveness, multiple health insurance organizations, lack of attention to all factors affecting health, inefficiency of evidence-based policy-making, and inefficiency regarding the proper enforcement of laws and regulations(34, 33). The health system governance requires interaction and cooperation between the health and non-health enterprises, the governmental and non-governmental sectors, and all citizens (33).Additionally, the term "sovereignty" must be defined and operationalized precisely (35); and health system governance's problems and challenges must be addressed(36).
Definition of good governance
Governance is one of the most fundamental demands of human communities, the importance of which no one can ignore. While there are significant disagreements, the majority of theorists are concerned with the administration of justice, avoidance of tyranny and absolutism, and the establishment of order and security. Good governance is a relatively recent phenomenon (37). It is the practice of managing a country's resources in order to fulfill desired goals. Good governance encompasses both the government, and the quality of its operations is characterized by the private sector and civil society's participation (1).
Good governance indicators
It is widely accepted that good governance is grounded on eight significant features such as, participation, agreement, responsiveness, transparency, accountability, effectiveness and efficacy, inclusiveness and equity, and the rule of law. More specifically, in good governance, all individuals (citizens) have the right to directly or indirectly be cooperative and express their opinions about making the decisions (i.e., participation) (7). Good governance also needs to mediate between perspectives and various interests of the society in order to achieve a widespread consensus on political values and the best interests of the whole community (i.e., consensus-oriented) (38). Furthermore, good governance should hold the decision-makers accountable for the process and organizations and find opportunities to serve them all (i.e., accountability) (39). The consequence of these processes and institutions is to meet the needs of the community while using the available resources efficiently (i.e., effectiveness and efficacy) (38, 7). Good governance should provide equal opportunities for all the citizens to progress, particularly the vulnerable (i.e., inclusiveness and equity). Another important element is effective legal framework for proper and impartial functioning. It needs to protect the individuals’ rights and have a strong judiciary and security system to enforce the laws effectively (i.e., rule of law) (7).
The Indicators of good governance in health system
Components such as painting a strategic perspective/vision, participation, consensus, the rule of law, transparency, accountability, equity and inclusiveness, efficiency and effectiveness, responsiveness, intelligence, information, and ethics necessitate further discussion in establishing good governance in the health system (40).
Good governance in health system
The main purpose of good governance is to save and make the best use of available resources in implementing the health system policies (41). The local or national governance models could be established considering the national and historical experiences as well as the cultural values of the country (36). It seems that motivation is a key factor in enforcing good governance by health providers in healthcare centers (42). The enforcement could be considerably successful, providing that the authorities or the implementers are encouraged and supported (43). The implementation of good governance in the health system could be highly advantageous for providing the high-quality and low-cost services. It may also satisfy the stakeholders in the health system, leading to transparency and accountability in this section (35). It is necessary for the public, private and civil sections to cooperate if they attempt to improve the quality of services in the health system (44). It is argued that the main components of governance in the Iranian health system are quality enhancement, management and leadership, community cooperation, the effectiveness of primary healthcare, security/safety, evaluation, healthcare audit, and health information management (45). The use of good governance both in the policy-making process and the implementation of the health policies could contribute to a tangible enhancement in the quality of services in the health system (36).
Recommendations to improve health policy-making cycle using good governance approach
1) Governmental measures associated with health and good health governance should be developed with a strong focus on health.
2) All policies are founded on the basis of higher well-established documents, justice, and sustainability. Justice in health system should be given careful consideration during the whole process policy-making. To achieve good governance along with the implementation of justice in health, it is essential that during the formulation of the preliminary actions and policy-making special attention be given to deprived and low-income areas, and those locating in special climates to provide them health services and distribute the available sources effectively.
3) Regarding health as a necessary aim to assess the health consequences of decisions in all domains of policy-making with special emphasis on justice perspective is accepted.
4) Prior to the policy-making stage, preliminary measures should be taken by organizing the intersectoral specialized groups in the policy-making, planning, budget allocation, resources assignment phases, and prioritizing are dealt with them in the light of good governance. Preparing checklists using the viewpoints of aforementioned groups in conjunction with the representatives of the intended correspondent organization including Insurance, Red Crescent, etc, ( the issues conveyed to the decision making body of health system) are prioritized according to justice, public advantage, responding to the needs, and dominance of the law.
5) Health system policy should follow clarity, dominance of rule, justice, effectiveness, efficiency, and cooperation along with sticking with policy-making principles.
6) Intersectoral cooperation is conceived as one of the most effective factors in implementing policies of the health system. The executing organizations should be identified in line with each policy. By planning appropriate governance indicators such as commitment, cooperation, effectiveness, and accountability, the role and duties of each organization are specified. For example, to supply medicine and import it to get rid of the crisis associated with COVID-19, the Ministry of Health should be in charge while the role and duties of other organizations, including Red Crescent, should be meticulously spelled out to the extent that they can be accountable.
7)All the required planning to implement formulated policy effectively should be specified and predicted by experts in planning and future research, encapsulating all levels of strategic planning, executing, and operating.
8) The required resources to implement the policy effectively are predicted, and the organization supplying these resources is meticulously determined. The required resources include human, , equipment, and pharmacy resources, and financial aspects which are devoted in the light of good governance principles.
9) Health services and the resources are revised so as to improve health and share the authority with other sections and fields regarding particular groups of people.
10) Effective implementation of the health system policies is attainable with the participation of the stakeholders such as the Retired Personnel Organization, members of parliament, Non-Governmental Organizations (NGO) along with good governance in the light of criteria such as participation, commitment, effectiveness, aggregation-orientation, and unanimity. In effect, people, as the main resources of health, are given more attention, and the total approach concerns social participation.
11) It is strongly recommended to draw upon the viewpoints of the professionals, specialized personnel, and managers who had more experience in implementing the policies of health system along with the knowledge and perspective of university professors, who possess the qualities of successful administrators. For instance, using the experience of those who successfully founded and implemented the health and treatment network can be really helpful in making and implementing the policy of family physicians.
12) Drawing on the experiences of international organizations and other countries regarding using good governance in health system policy-making should be done with localization in mind.
13) The evaluation should be informative and constant not only in policy evaluation but also in all the health system policy-making. The evaluation should be done in the light of criteria such as justice, rule dominancy, clarity, and accountability. Furthermore, it can be carried out locally and internationally.
14) Implementing the indicators of good governance should be regarded as a long-term strategy not restricted to a short-term and temporary plan.
15) Instead of viewing good governance as a challenge, high-ranking officials should consider it an opportunity.
16) Changing the attitudes with regard to good governance denotes that social activists should raise their awareness; there is no interaction between good governance and tradition. Besides, good governance should be administered to manage the society better and create dynamicity.
17) Policy-making cycle along with health system governance can be improved in the light of implementing good governance.
Discussion
Many studies have been carried out on the topic of this research. A number of nationwide studies have turned to the methods and principles of good governance. Furthermore, a number of international studies have investigated health system and its association with principles of good governance. Despite the numerous studies related to implementing policies of the health system along with identifying the barriers and proposing some guidelines, models, and strategies, they have not had any positive effect on policy-making and implementation. There are a number of possible justifications for this gap. If identifying the problems of policy-making are only restricted to and done within the Ministry of Health without considering the status and authority of high-ranking officials and duties of other organizations, the implementation stage will encounter problems and may result in failure. Besides its leading role in the health policy with regard to supplying financial support and providing the services, health system should cooperate with other sections in a complicated and multi-faceted environment for development (14). Undermining or neglecting these factors can pose a serious challenge to implementing these policies (20). In some studies, the importance of prioritizing in policy-making has been stressed (16). Unless the priorities in the health system and even the general priorities of the government are taken into account, a large number of proposed plans cannot satisfy and cover the basic needs, and accordingly, leads to wasting the resources, reconstruction, and even failure in achieving the goals. International support for the importance of a comprehensive, widespread, and multi-faceted outlook that takes into account all local, regional, national, and international indicators in policy-making was emphasized in a number of studies (20). Policy-making by means of shedding light on the plans requiring international support is an influential step in the successful implementation of these policies. In some studies, the necessity of health in all policies has been emphasized (18). For this matter, the awareness of citizens on general health should be raised, trained personnel should be employed in various domains, and a team should be formed with members possessing the required skill, comprehensive knowledge, and innovation. There is also a need for international support from international organizations along with equal distribution of the benefits (financial or non-financial). Employing various researchers, academic institutes, and health-related research without consideration for political matters or financial accountability compatible with the plans can give sufficient grounds for successful implementation (27). Policy-making should be based on the studies done (46). Based on various studies, university centers, studies related to the health domain without considering political matters and financial accountability consistent with the plans can provide strong bases for successful implementation of the policies (36). Strengthening the technical potential of the studies, better classification of research findings, using social networks, and establishing research centers in the Ministry of Health aimed to improve health system dominance, along with the effective implementation of the policies, are really effective measures. Attracting the participation of stakeholders, social accountability, implementation warranty, meritocracy, permanent position, using scientific documentation, cooperation capacity, and coordination in installing health database all play a major role in proper implementation (47). Stakeholders and role creators can play a crucial role in controlling the changes and improving the quality of the content of health policy in the future (48). Health policymakers in Iran should pursue the goals in such a way that modifications, on a smaller scale, be based on a comprehensive model incorporating social, political, economic factors and with the cooperation of stakeholders (49). Realizing health system policies is not possible without the cooperation of stakeholders and relevant organizations. Furthermore, given the studies done in conjunction with well-established documents on the basis of local, regional, cultural, and climatic conditions, the planning process in health policy-making should be done regionally according to the conditions and situation of that region. Intersectoral actions in the health domain, appropriate general policies, and health in all policies are the three main waves of policy-making which, in conjunction with the change in political paradigm, have provided a new perspective in health system governance (50).Given the significance of the health along with complexities in this domain, modification in governance perspective and delving into good governance seem to be a necessity. Governance is not an intervention but a value system and a kind of reflection and a socio-cultural belief toward development, bringing about some opportunities for health and decreasing inequality. In addition, the participatory approach has emphasized the intersectoral cooperation, meta-sectoral health coordination, and improved systemic qualities of general policy-making, and, at the same time, resulted in effective plans in all political sections (51). Achieving such goals from the coordinated governance for health, calls for political willingness and implementation of good governance in the process of health policy-making. Policy-making process in the health system is a widespread and comprehensive practice in all stages in which one needs to make use of legal means, the intergovernmental, international and private organizations, elites, researchers, and the experience of other countries (52). Formulation of the conceptual model for policy-making with the good governance approach on behalf of policymakers can play an important part in this regard. Health system governance has encountered various challenges (1); by improving the approach mentioned, policymakers in the can make a great contribution to improve the function of the health system. Taking the example of and localizing the administrative indicators of the health system in successful countries can strengthen the system and provide enough grounds to achieve sustainable goals, and finally, improve the health system of the country. Formulation of the policy depends upon its type. Therefore, the same model cannot be drawn upon to formulate it (53). Each policy depends on its means and support from different organizations. At the same time, it is in line with appropriate domestic and foreign situations to achieve successful implementation. Improving the implementation quality of formulated policies in different levels of the country's health system results in mutual trust between the health system and different levels of the target society. This creates motivation, and encourages cooperation, of implementers, along with providing desirable provisions to actualize creativity in implementing the policies, improving health indices in the country, and with regard to the validity of the health system (36). Accordingly, some changes need to be made regarding good governance for health system. Investigating the possible gaps associated with leadership, supervision measures, technical capacities for planning and managing health system, and methods of financial implementation can positively affect the trends in continuous development and enforcement of preliminary health care measures (54). Investigating and identifying barriers can result in correcting present trends in implementing the policies and organizational learning; thus, removing the current barriers for future policy-making. There is also a lack of political commitment and resource (55). The dominance of indicators for good governance in policy-making process and constant supervision can promote good governance in the health system. The constituent elements of good governance are applied as a measurement tool for governance conditions in different countries, and the intended countries are assessed based on previously specified indicators. This possesses a high degree of acceptability. The World Bank investigates the governance status of different countries and, afterward, announces the report officially (56). This report can be the main basis for most decisions, judgment, and internal and external discussions. Accordingly, using and applying good governance is really effective in the success and possible failure of many countries. Health governance is a complicated and multi-faceted process. A look at the trends in governance and its use in the health system by the governments aiming to promote health care indicated that a multi-leveled which benefits many people, is required to guard against current and emergent problems in general health (57). Developing a model for policy-making is just attainable by good governance. It is crystal clear that the current study, like other studies, suffers from some limitations. There were few studies associated with this study in developing countries and those adopting the similar health system dominant in Iran. Like other review studies, the intended articles were taken from main national and international databases. Any possible attempt was made to use the studies that could cover the inclusion and exclusion criteria. However, there are some unpublished articles, which can be regarded as a possible limitation of review articles. Given the fact that there were no similar studies, the findings can be viewed as positive steps with regard to the health system policy in Iran. This can be considered a strong point of the present study and the recommendations are intended to strengthen the policy-making cycle and achieve the desired results. These considerations might serve as evidence of the novelty of this research project.
Conclusion
Strengthening health governance guarantees the desired results of health policy-making for the people. Therefore, designing a policy-making process model with a good governance approach is integral to the success of the development of the health system. Considering the legal mission of the Supreme Council of Health and Food Security (the highest policy-making authority in the Ministry of Health), it is recommended that the Council implement the practical recommendations of this research in incorporating the good governance approach into the health policy-making cycle.
Acknowledgments
The authors would like to thank everyone who contributed to undertaking this research.
Conflict of interest
The authors declared no conflict of interest.
Funding
This research did not receive any grant from a funding agency.
Ethical considerations
This article is an excerpt from a PhD dissertation on public management (a subfield of public policy-making) that was authorized by the Islamic Azad University of Gorgan (Iran country) on 2021/7/18 under the code 162280383.
Code of Ethics
162280383
Authors' contributions
M.A and A.V.M, Contributed to the study concept and design; M.A, Data collection; M.A and A.V.M, Participated in collecting analysis, and interpretation of data; M.A and A.V.M, Article writing and Revision of the article; A.F.M, Review of draft article. All authors read and approved the final manuscript.
Open Access Policy
JCHR does not charge readers and their institution for access to its papers. Full text download of all new and archived papers are free of charge.
Health policy-making
Identifying issues and developing evidence-based models of problems, bringing other organizations together according to their responsibilities, looking for support to solve problems, soliciting new ideas and mediating and negotiating to achieve a policy plan, prioritizing policy design, and managing the policy process are among the Ministry of Health's most important responsibilities. These responsibilities are consistent with the policy-making process (12). Management of the health system will take place across all sectors and levels, despite their structural differences (13). The decisions made must be enforceable, frequently monitored, and modified if necessary. Moreover, the Ministry of Health must be capable of mobilizing resources and resolving problems via the engagement of all stakeholders and government agencies associated with health, as well as integrating the experience and recommendations from professionals in this field (12). The policy-making process is discussed in detail in the majority of the extracted articles as problem identification, policy formulation, policy implementation, and performance evaluation (14). This process is the same in the majority of countries. Policymakers in government organizations can use an analytical system and expert committees to address the policy-making process by removing human and organizational constraints and implementing a comprehensive model (13). Several critical points should be taken into consideration, which include determining the root cause of the problem, formulating a policy based on previous evaluations, maintenance, performance monitoring, evaluating the process in which the problem occurs, and final evaluation (15). The role of policymakers is extremely important, as is their capacity to understand the organization's values, unify those involved in this sector, and utilize all the aspects involved in policy-making (16). Policymakers play a more important role in the health system than other organizations (17). Policy formulation and implementation occurs following the collection of evidence and consultation with stakeholders (18). Prioritization is an extremely crucial element (19). Focusing on health prioritization is important due to the lack of resources and the need for appropriate resource allocation, the complexity, and dispersion of health care providers, and uncertainty and rapid change. It is worth noting that adaptability occurs more readily when managers and leaders have a clear orientation, strategy, and coordination in this regard (20). In the spirit of the complications and significance of health policy-making, planning for policy implementation is of paramount significance (16). Globalization and decentralization, the involvement of social media, and pressure groups in the policy-making process are important (18). International support is another aspect in policy-making (20). The political and social structure of countries has a major effect in policy-making (17). The influence of political communication and the form of government on policy-making demonstrates the prevalence of health in all policies (20). In addition, using research and evidence in policy marking is vital (21). Policy formulation depends on its type; hence, one framework or model cannot always be utilized for all kinds of policies (14). Political, economic, and social structures also play a role in policy-making; although, the success of policy-making rests solely on what occurs in practice (e.g., practical considerations) (22). Through workshops and national education programs, the importance of managers participating in the formulation process and considering high-level policy documents should be emphasized for optimal policy-making (23). Successful organizations are those that can implement what they formulate (24). It is recommended that stakeholders receive feedback on implementation issues (25). A large body of research has revealed a variety of operational barriers. The following factors have been identified as contributing to policy-making failures in the majority of investigations.; the complexities and lack of transparency surrounding policies and programs, the time and energy spent formulating them, the inaccuracy with which constraints and obstacles are identified, the lack of recognition and transparency surrounding departmental responsibilities and communication with organizations outside of health agencies and collaboration in this area, Stakeholders' uninvolvement in the formulation process, which frequently results in implementation gaps, the lack of appropriate financial resources, and the focus of the majority of ministries on operations in specific communities such as hospital services or on illnesses and conflicts in daily crisis management (26). The main motives for health policy failure or success are incomprehension of the policy formulation process, identification of the impact and the role of each of the players involved, and ultimately an attempt to balance these factors, particularly in relation to the power of several key players. It is in such a way that the failure of some policies to achieve their objectives can be attributed to disregarding some of the factors influencing the analysis stage (26). Other factors contributing to the failure of some programs include policymakers' lack of knowledge about research procedures and their inability to employ research in health policy-making (27). The majority of studies recommended the proliferation of a model for the health system's policy-making process, which would encompass the preliminaries steps for the formulation, implementation, evaluation, and sustainability of policy products. Several studies addressed the evolution of health system governance and the move toward a more contemporary perception of good governance.
Health system governance
Sovereignty or governance refers to a collection of government-imposed laws and regulations which must be enforced by government agents (28, 29). The purpose of governance is to design an appropriate structure for achieving organizational goals, select and appoint individuals within the organizations, formulate policies and regulations, determine the organization's strategic direction, manage resources necessary to implement policies, ensure the implementation of high-level rules, and supervise, monitor and control the organization's performance (30, 31). Developing countries confront challenges in health system governance. Many of these challenges lack knowledge and skills in health policy formulation and management, participation of all stakeholders in health policy formulation, and might fail to pay attention to all factors affecting health. They may also lack an incoherent approach to the health formulation process, have an ineffective leadership regarding health reform, and not implement all rules and regulations and periodically evaluate them (32). Iran's health system governance is also confounded by challenges, including the overlapping health system and other executive organizations responsibilities, unsatisfactory implementation of the structure approved by the Ministry of Health, lack of transparency regarding individual responsibilities, authority, and responsiveness, multiple health insurance organizations, lack of attention to all factors affecting health, inefficiency of evidence-based policy-making, and inefficiency regarding the proper enforcement of laws and regulations(34, 33). The health system governance requires interaction and cooperation between the health and non-health enterprises, the governmental and non-governmental sectors, and all citizens (33).Additionally, the term "sovereignty" must be defined and operationalized precisely (35); and health system governance's problems and challenges must be addressed(36).
Definition of good governance
Governance is one of the most fundamental demands of human communities, the importance of which no one can ignore. While there are significant disagreements, the majority of theorists are concerned with the administration of justice, avoidance of tyranny and absolutism, and the establishment of order and security. Good governance is a relatively recent phenomenon (37). It is the practice of managing a country's resources in order to fulfill desired goals. Good governance encompasses both the government, and the quality of its operations is characterized by the private sector and civil society's participation (1).
Good governance indicators
It is widely accepted that good governance is grounded on eight significant features such as, participation, agreement, responsiveness, transparency, accountability, effectiveness and efficacy, inclusiveness and equity, and the rule of law. More specifically, in good governance, all individuals (citizens) have the right to directly or indirectly be cooperative and express their opinions about making the decisions (i.e., participation) (7). Good governance also needs to mediate between perspectives and various interests of the society in order to achieve a widespread consensus on political values and the best interests of the whole community (i.e., consensus-oriented) (38). Furthermore, good governance should hold the decision-makers accountable for the process and organizations and find opportunities to serve them all (i.e., accountability) (39). The consequence of these processes and institutions is to meet the needs of the community while using the available resources efficiently (i.e., effectiveness and efficacy) (38, 7). Good governance should provide equal opportunities for all the citizens to progress, particularly the vulnerable (i.e., inclusiveness and equity). Another important element is effective legal framework for proper and impartial functioning. It needs to protect the individuals’ rights and have a strong judiciary and security system to enforce the laws effectively (i.e., rule of law) (7).
The Indicators of good governance in health system
Components such as painting a strategic perspective/vision, participation, consensus, the rule of law, transparency, accountability, equity and inclusiveness, efficiency and effectiveness, responsiveness, intelligence, information, and ethics necessitate further discussion in establishing good governance in the health system (40).
Good governance in health system
The main purpose of good governance is to save and make the best use of available resources in implementing the health system policies (41). The local or national governance models could be established considering the national and historical experiences as well as the cultural values of the country (36). It seems that motivation is a key factor in enforcing good governance by health providers in healthcare centers (42). The enforcement could be considerably successful, providing that the authorities or the implementers are encouraged and supported (43). The implementation of good governance in the health system could be highly advantageous for providing the high-quality and low-cost services. It may also satisfy the stakeholders in the health system, leading to transparency and accountability in this section (35). It is necessary for the public, private and civil sections to cooperate if they attempt to improve the quality of services in the health system (44). It is argued that the main components of governance in the Iranian health system are quality enhancement, management and leadership, community cooperation, the effectiveness of primary healthcare, security/safety, evaluation, healthcare audit, and health information management (45). The use of good governance both in the policy-making process and the implementation of the health policies could contribute to a tangible enhancement in the quality of services in the health system (36).
Recommendations to improve health policy-making cycle using good governance approach
1) Governmental measures associated with health and good health governance should be developed with a strong focus on health.
2) All policies are founded on the basis of higher well-established documents, justice, and sustainability. Justice in health system should be given careful consideration during the whole process policy-making. To achieve good governance along with the implementation of justice in health, it is essential that during the formulation of the preliminary actions and policy-making special attention be given to deprived and low-income areas, and those locating in special climates to provide them health services and distribute the available sources effectively.
3) Regarding health as a necessary aim to assess the health consequences of decisions in all domains of policy-making with special emphasis on justice perspective is accepted.
4) Prior to the policy-making stage, preliminary measures should be taken by organizing the intersectoral specialized groups in the policy-making, planning, budget allocation, resources assignment phases, and prioritizing are dealt with them in the light of good governance. Preparing checklists using the viewpoints of aforementioned groups in conjunction with the representatives of the intended correspondent organization including Insurance, Red Crescent, etc, ( the issues conveyed to the decision making body of health system) are prioritized according to justice, public advantage, responding to the needs, and dominance of the law.
5) Health system policy should follow clarity, dominance of rule, justice, effectiveness, efficiency, and cooperation along with sticking with policy-making principles.
6) Intersectoral cooperation is conceived as one of the most effective factors in implementing policies of the health system. The executing organizations should be identified in line with each policy. By planning appropriate governance indicators such as commitment, cooperation, effectiveness, and accountability, the role and duties of each organization are specified. For example, to supply medicine and import it to get rid of the crisis associated with COVID-19, the Ministry of Health should be in charge while the role and duties of other organizations, including Red Crescent, should be meticulously spelled out to the extent that they can be accountable.
7)All the required planning to implement formulated policy effectively should be specified and predicted by experts in planning and future research, encapsulating all levels of strategic planning, executing, and operating.
8) The required resources to implement the policy effectively are predicted, and the organization supplying these resources is meticulously determined. The required resources include human, , equipment, and pharmacy resources, and financial aspects which are devoted in the light of good governance principles.
9) Health services and the resources are revised so as to improve health and share the authority with other sections and fields regarding particular groups of people.
10) Effective implementation of the health system policies is attainable with the participation of the stakeholders such as the Retired Personnel Organization, members of parliament, Non-Governmental Organizations (NGO) along with good governance in the light of criteria such as participation, commitment, effectiveness, aggregation-orientation, and unanimity. In effect, people, as the main resources of health, are given more attention, and the total approach concerns social participation.
11) It is strongly recommended to draw upon the viewpoints of the professionals, specialized personnel, and managers who had more experience in implementing the policies of health system along with the knowledge and perspective of university professors, who possess the qualities of successful administrators. For instance, using the experience of those who successfully founded and implemented the health and treatment network can be really helpful in making and implementing the policy of family physicians.
12) Drawing on the experiences of international organizations and other countries regarding using good governance in health system policy-making should be done with localization in mind.
13) The evaluation should be informative and constant not only in policy evaluation but also in all the health system policy-making. The evaluation should be done in the light of criteria such as justice, rule dominancy, clarity, and accountability. Furthermore, it can be carried out locally and internationally.
14) Implementing the indicators of good governance should be regarded as a long-term strategy not restricted to a short-term and temporary plan.
15) Instead of viewing good governance as a challenge, high-ranking officials should consider it an opportunity.
16) Changing the attitudes with regard to good governance denotes that social activists should raise their awareness; there is no interaction between good governance and tradition. Besides, good governance should be administered to manage the society better and create dynamicity.
17) Policy-making cycle along with health system governance can be improved in the light of implementing good governance.
Discussion
Many studies have been carried out on the topic of this research. A number of nationwide studies have turned to the methods and principles of good governance. Furthermore, a number of international studies have investigated health system and its association with principles of good governance. Despite the numerous studies related to implementing policies of the health system along with identifying the barriers and proposing some guidelines, models, and strategies, they have not had any positive effect on policy-making and implementation. There are a number of possible justifications for this gap. If identifying the problems of policy-making are only restricted to and done within the Ministry of Health without considering the status and authority of high-ranking officials and duties of other organizations, the implementation stage will encounter problems and may result in failure. Besides its leading role in the health policy with regard to supplying financial support and providing the services, health system should cooperate with other sections in a complicated and multi-faceted environment for development (14). Undermining or neglecting these factors can pose a serious challenge to implementing these policies (20). In some studies, the importance of prioritizing in policy-making has been stressed (16). Unless the priorities in the health system and even the general priorities of the government are taken into account, a large number of proposed plans cannot satisfy and cover the basic needs, and accordingly, leads to wasting the resources, reconstruction, and even failure in achieving the goals. International support for the importance of a comprehensive, widespread, and multi-faceted outlook that takes into account all local, regional, national, and international indicators in policy-making was emphasized in a number of studies (20). Policy-making by means of shedding light on the plans requiring international support is an influential step in the successful implementation of these policies. In some studies, the necessity of health in all policies has been emphasized (18). For this matter, the awareness of citizens on general health should be raised, trained personnel should be employed in various domains, and a team should be formed with members possessing the required skill, comprehensive knowledge, and innovation. There is also a need for international support from international organizations along with equal distribution of the benefits (financial or non-financial). Employing various researchers, academic institutes, and health-related research without consideration for political matters or financial accountability compatible with the plans can give sufficient grounds for successful implementation (27). Policy-making should be based on the studies done (46). Based on various studies, university centers, studies related to the health domain without considering political matters and financial accountability consistent with the plans can provide strong bases for successful implementation of the policies (36). Strengthening the technical potential of the studies, better classification of research findings, using social networks, and establishing research centers in the Ministry of Health aimed to improve health system dominance, along with the effective implementation of the policies, are really effective measures. Attracting the participation of stakeholders, social accountability, implementation warranty, meritocracy, permanent position, using scientific documentation, cooperation capacity, and coordination in installing health database all play a major role in proper implementation (47). Stakeholders and role creators can play a crucial role in controlling the changes and improving the quality of the content of health policy in the future (48). Health policymakers in Iran should pursue the goals in such a way that modifications, on a smaller scale, be based on a comprehensive model incorporating social, political, economic factors and with the cooperation of stakeholders (49). Realizing health system policies is not possible without the cooperation of stakeholders and relevant organizations. Furthermore, given the studies done in conjunction with well-established documents on the basis of local, regional, cultural, and climatic conditions, the planning process in health policy-making should be done regionally according to the conditions and situation of that region. Intersectoral actions in the health domain, appropriate general policies, and health in all policies are the three main waves of policy-making which, in conjunction with the change in political paradigm, have provided a new perspective in health system governance (50).Given the significance of the health along with complexities in this domain, modification in governance perspective and delving into good governance seem to be a necessity. Governance is not an intervention but a value system and a kind of reflection and a socio-cultural belief toward development, bringing about some opportunities for health and decreasing inequality. In addition, the participatory approach has emphasized the intersectoral cooperation, meta-sectoral health coordination, and improved systemic qualities of general policy-making, and, at the same time, resulted in effective plans in all political sections (51). Achieving such goals from the coordinated governance for health, calls for political willingness and implementation of good governance in the process of health policy-making. Policy-making process in the health system is a widespread and comprehensive practice in all stages in which one needs to make use of legal means, the intergovernmental, international and private organizations, elites, researchers, and the experience of other countries (52). Formulation of the conceptual model for policy-making with the good governance approach on behalf of policymakers can play an important part in this regard. Health system governance has encountered various challenges (1); by improving the approach mentioned, policymakers in the can make a great contribution to improve the function of the health system. Taking the example of and localizing the administrative indicators of the health system in successful countries can strengthen the system and provide enough grounds to achieve sustainable goals, and finally, improve the health system of the country. Formulation of the policy depends upon its type. Therefore, the same model cannot be drawn upon to formulate it (53). Each policy depends on its means and support from different organizations. At the same time, it is in line with appropriate domestic and foreign situations to achieve successful implementation. Improving the implementation quality of formulated policies in different levels of the country's health system results in mutual trust between the health system and different levels of the target society. This creates motivation, and encourages cooperation, of implementers, along with providing desirable provisions to actualize creativity in implementing the policies, improving health indices in the country, and with regard to the validity of the health system (36). Accordingly, some changes need to be made regarding good governance for health system. Investigating the possible gaps associated with leadership, supervision measures, technical capacities for planning and managing health system, and methods of financial implementation can positively affect the trends in continuous development and enforcement of preliminary health care measures (54). Investigating and identifying barriers can result in correcting present trends in implementing the policies and organizational learning; thus, removing the current barriers for future policy-making. There is also a lack of political commitment and resource (55). The dominance of indicators for good governance in policy-making process and constant supervision can promote good governance in the health system. The constituent elements of good governance are applied as a measurement tool for governance conditions in different countries, and the intended countries are assessed based on previously specified indicators. This possesses a high degree of acceptability. The World Bank investigates the governance status of different countries and, afterward, announces the report officially (56). This report can be the main basis for most decisions, judgment, and internal and external discussions. Accordingly, using and applying good governance is really effective in the success and possible failure of many countries. Health governance is a complicated and multi-faceted process. A look at the trends in governance and its use in the health system by the governments aiming to promote health care indicated that a multi-leveled which benefits many people, is required to guard against current and emergent problems in general health (57). Developing a model for policy-making is just attainable by good governance. It is crystal clear that the current study, like other studies, suffers from some limitations. There were few studies associated with this study in developing countries and those adopting the similar health system dominant in Iran. Like other review studies, the intended articles were taken from main national and international databases. Any possible attempt was made to use the studies that could cover the inclusion and exclusion criteria. However, there are some unpublished articles, which can be regarded as a possible limitation of review articles. Given the fact that there were no similar studies, the findings can be viewed as positive steps with regard to the health system policy in Iran. This can be considered a strong point of the present study and the recommendations are intended to strengthen the policy-making cycle and achieve the desired results. These considerations might serve as evidence of the novelty of this research project.
Conclusion
Strengthening health governance guarantees the desired results of health policy-making for the people. Therefore, designing a policy-making process model with a good governance approach is integral to the success of the development of the health system. Considering the legal mission of the Supreme Council of Health and Food Security (the highest policy-making authority in the Ministry of Health), it is recommended that the Council implement the practical recommendations of this research in incorporating the good governance approach into the health policy-making cycle.
Acknowledgments
The authors would like to thank everyone who contributed to undertaking this research.
Conflict of interest
The authors declared no conflict of interest.
Funding
This research did not receive any grant from a funding agency.
Ethical considerations
This article is an excerpt from a PhD dissertation on public management (a subfield of public policy-making) that was authorized by the Islamic Azad University of Gorgan (Iran country) on 2021/7/18 under the code 162280383.
Code of Ethics
162280383
Authors' contributions
M.A and A.V.M, Contributed to the study concept and design; M.A, Data collection; M.A and A.V.M, Participated in collecting analysis, and interpretation of data; M.A and A.V.M, Article writing and Revision of the article; A.F.M, Review of draft article. All authors read and approved the final manuscript.
Open Access Policy
JCHR does not charge readers and their institution for access to its papers. Full text download of all new and archived papers are free of charge.
References
1. Mosadeghrad AM, Rahimi-Tabar P. Health system governance in Iran: A comparative study. Razi Journal of Medical Sciences. 2019; 26(9): 10-28. [Persian]
2. Joulaei H, Bagheri-Lankarani K, Zarei N, et al. Stewardship and its role in Iran'shealthsystem: A scoping review. IJHP. 2018; 2: 206-16. [Persian]
3. World Health Organization. Government of South Australia. Adelaide statement on health in all policies. 2010. doi: 10.1093/heapro/daq034.
4. De Leeuw E, Kickbusch I, Palmer N, et al. European Healthy Cities come to terms with health network governance. Health promotion international. 2015; 30(suppl_1): i32-44. doi: 10.1093/heapro/dav040.
5. Alamdari S, Alamdari A. IR Iran national health system strategic architecturing based on national vision 1404: A proposed model. Iranian Journal of Public Policy. 2015; 1(1): 21-42. doi: 10.22059/ppolicy.2015.57150. [Persian]
6. Ebrahimpour H, Eliki F. Investigating the role of good governance in the efficiency of governments. InInternational Conference of Management Elites, Iran; Tehran. 2016; 1. [Persian]
7. Sharifzadeh F, Rahmarallah G. Good governance and the role of government. organizational culture management. 2003; 1(4): 93-109. [Persian]
8. Rahmani K, Rezayatmand R, Sadeghpour N, et al. Policy-making for rationing in the healthcare system: a review to provide suggestions for Iran. Management Strategies in Health System. 2018; 3(3): 249-62. [Persian]
9. Mosadeghrad AM. An integrated health policy making and analysis model. Tehran Univ Med J. 2020; 77(12): 791. [Persian]
10. O’Brien BC, Harris IB, Beckman TJ, et al. Standards for reporting qualitative research: a synthesis of recommendations. Academic medicine. 2014; 89(9): 1245-51.
11. Hong QN, Fàbregues S, Bartlett G, et al. The Mixed Methods Appraisal Tool (MMAT) version 2018 for information professionals and researchers. Education for information. 2018; 34(4): 285-91.
12. Zazerani Y, Reza M. Understanding the Policy Process; an Overview of the Concepts, Theories, and Models of Policy Process. Iranian Journal of Public Policy. 2018; 3(4): 189-202. [Persian]
13. Shankardass K, Muntaner C, Kokkinen L, et al. The implementation of Health in All Policies initiatives: a systems framework for government action. Health research policy and systems. 2018; 16(1): 1-0. doi: https://doi.org/10.1186/s12961-018-0295-z
14. Strehlenert H, Richter-Sundberg L, Nyström ME, et al. Evidence-informed policy formulation and implementation: a comparative case study of two national policies for improving health and social care in Sweden. Implementation Science. 2015; 10: 1-0. doi: 10.1186/s13012-015-0359-1.
15. Babaei S, Tavakoli G. A policy making process model for public organizations. Public Policy 2015; 1(3): 29-53. doi: 10.22059/ppolicy.2015.57678. [Persian]
16. Maher A, Maziar P. Health policy making process: a systematic review article, Shahid Beheshti University of Medical Sciences, Tehran, Iran. [Persian]
17. Azline A, Iszaid I, Syahira S, et al. Policy arena of health policy-making process in developing countries. International Journal of Public Health and Clinical Sciences 2018; 5(3): 32-48.
18. Ministry of Social Affairs and Health of Finland, in collaboration with the National Institute for Health and Welfare of Finland (THL), the European Observatory on Health Systems and Policies, and the United Nations Research Institute for Social Development (UNRISD). Health in all policies: seizing opportunities, implementing policies; Finland. 2013; 25-287.
19. Zuckerman AM. Successful strategic planning for a reformed delivery system. Journal of Healthcare Management. 2014; 59(3): 168-72.
20. Kokkinen L, Muntaner C, O’Campo P, et al. Implementation of Health 2015 public health program in Finland: a welfare state in transition. Health Promotion International. 2019; 34(2): 258-68.
21. Uneke CJ, Ezeoha AE, Ndukwe CD, et al. Research priority setting for health policy and health systems strengthening in Nigeria: the policymakers and stakeholders perspective and involvement. Pan African Medical Journal. 2014; 16(1).
doi:10.11604/pamj.2013.16.10.2318.
22. Damari BA, Monazzam K, Salarianzadeh H. Where and how to make wise policies for health? A qualitative study on the characteristics of health policy system in the Islamic Republic of Iran. Hakim Journal. 2011; 13(4): 210-8. [Persian]
23. Nasrollapour-Shirvani SD, Motlagh ME, Shariati M, et al. The Strategic Plan of Iranian Medical Sciences Universities: From Theory to Practice. Health Information Management. 2016; 12(6): 770-6. [Persian]
24. Alam AY, Alabdulaali MK. Hospital vision and mission strategic planning and departmental performance. J Pak Med Assoc. 2015; 65: 345-46.
25. Bowen G, Bowen D. Strategy formulation and uncertainty in environments. Journal of Business and Economics. 2014; 5(12): 2315-26. doi: 10.15341/jbe(2155-7950)/12.05.2014/012.
26. Gholipor R, Mafimoradi S, Rahnavard F, et al. Systematic Analysis of Research Articles on Health Policy in the Developing Countries: Implications for Researchers. Journal of Iranian Public Administration Studies. 2019; 2(2): 25-45. doi: 10.22034/jipas.2019.91495. [Persian]
27. Hyder AA, Corluka A, Winch PJ, et al. National policy-makers speak out: are researchers giving them what they need?. Health policy and planning. 2011; 26(1): 73-82. doi: 10.1093/heapol/czq020.
28. Mafimoradi S, Gholipour R, Rahnavard F, et al. How Health Policies change in Islamic Republic of Iran? A substantive theory to understand the policy process. Payesh (Health Monitor). 2020; 19(6): 673-91. doi: 10.29252/payesh.19.6.673. [Persian]
29. Mosadeghrad AM, Rahimi-Tabar P. Health system governance in Iran: A comparative study. Razi Journal of Medical Sciences. 2019; 26(9): 10-28. [Persian]
30. World Health Organization. Everybody’s business: strengthening health systems to improve health outcomes: WHO’s framework for action. Production. 2007: 1-56.
31. Davies C. Links between Governance, Incentives and Outcomes: A Review of the Literature National Co-ordinating Centre for NHS Service Delivery and Organisation R&D. London: The Stationery Office. 2005.
32. World Health Organization. Governance for Health in the 21st Century. WHO Europe; 2012.
33. Lankarani KB, Alavian SM, Peymani P. Health in the Islamic Republic of Iran, challenges and progresses. Medical journal of the Islamic Republic of Iran. 2013; 27(1): 42.
34. Moghadam AV,Damari B, Alikhani S, et al. Health in the 5 th 5-years development plan of Iran: main challenges,general policies and strategies. Iran J Public Health. 2013; 42(1): 42–49. [Persian]
35. Jafari F, HajiNabi K, Jahangiri K, et al. Good governance in the health system: A qualitative study. International Transaction Journal of Engineering, Management, & Applied Sciences & Technologies. 2019; 8: 1127-41. [Persian]
36. Saltman RB, Duran A. Governance, government, and the search for new provider models. International journal of health policy and management. 2016; 5(1): 33.
37. Emami M, Shakeri H. Good governance and The constitution of the Islamic Republic of Iran. Journal of Comparative Law. 2015; 1(2): 25-57. [Persian]
38. Alvaani SM, Alizadeh Saani M. Analyzing the Quality of Good Governance in Iran. Management Studies in Development and Evolution. 2007; 18(53): 1-24. [Persian]
39. Taqvaei AA, Tajdar R. An introduction to good urban governance in an analytical approach. Urban Management. 2009; 23(1): 45-58.
40. Maesoumi Z, Sanei M, Hematian H. A model for effective implementation of health policy in Iran. Quarterly Journal of Management Strategies in Health System. 2019; 4(2): 125-35. [Persian]
41. Afrasiabi, M. Indicators of good governance in the health system [M.Sc. thesis]. Iran. Islamic Azad University Safadasht; 2017. [Persian]
42. Pinterič U. Rethinking public policies Faculty of Organization Studies: Slovenia, Nova Mesto. 2014: 7-75.
43. Houngbo PT, Coleman HL, Zweekhorst M, et al. A model for good governance of healthcare technology management in the public sector: learning from evidence-informed policy development and implementation in Benin. PloS one. 2017; 12(1): e0168842.
44. Valera Mt, Hartigan-Go Ky, Visperas Mk. A Framework to Promote Good Governance in Healthcare.
45. Tabrizi JS, Pourasghar F, Nikjoo RG. Governance of iranian primary Health Care System: perceptions of experts. Iranian Journal of Public Health. 2019; 48(3): 541. [Persian]
46. El-Jardali F, Lavis JN, Ataya N, et al. Use of health systems evidence by policymakers in eastern Mediterranean countries: views, practices, and contextual influences. BMC health services research. 2012; 12(1): 1-20.
47. Jönsson K, Phoummalaysith B, Wahlström R, et al. Health policy evolution in Lao People’s Democratic Republic: context, processes and agency. Health policy and planning. 2015; 30(4): 518-27.
48. Khankeh HR, Lankarani KB, Zarei N, et al. Three decades of healthcare system reform in Iran from the perspective of universal health coverage: A macro-qualitative study. Iranian Journal of Medical Sciences. 2021; 46(3): 198. [Persian]
49. Malek Mohammadi HR, Vahdaninia V. The evolution of health policy: Transition to the governance paradigm for health. Iranian Journal of Public Policy. 2016; 2(2): 73-94. [Persian]
50. Vahdaninia V, Vosoogh Moghaddam A. Understanding late logic of health policy making: The transition to governance for health. Payesh (Health Monitor). 2018; 17(6): 631-46. [Persian]
51. Greer S, Wismar M, Figueras J. EBOOK: strengthening health system governance: better policies, stronger performance. McGraw-Hill Education (UK); 2015.
52. Cabral-Bejarano MS, Nigenda G, Arredondo A, et al. Stewardship and governance: structuring dimensions for implementation primary health care policies in Paraguay, 2008-2017. Ciência & Saúde Coletiva. 2018; 23: 2229-38.
53. Escobar-Ballesta M, García-Ramírez M, De Freitas C. Taking stock of Roma health policies in Spain: lessons for health governance. Health Policy. 2018; 122(4): 444-51.
54. Atun R. Transforming Turkey's health system—lessons for universal coverage. New England Journal of Medicine. 2015; 373(14): 1285-9.
55. Nicholson C, Hepworth J, Burridge L, et al. Translating the elements of health governance for integrated care from theory to practice: a case study approach. International Journal of Integrated Care. 2018; 18(1).
56. Liu SX, de Bont C. Barriers to strategic design: A perspective from China. She Ji: The Journal of Design, Economics, and Innovation. 2017; 3(2): 133-45.
57. Purehtesham M. Studying the effect of governance quality on health indicators in the countries of South-Western Asia. Social Welfare Quarterly. 2018; 18(69): 184-59.
Review: Review |
Subject:
Health care management
Received: 2023/02/9 | Accepted: 2023/04/16 | Published: 2023/11/28
Received: 2023/02/9 | Accepted: 2023/04/16 | Published: 2023/11/28
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution 4.0 International License. |