Volume 12, Issue 2 (11-2023)
JCHR 2023, 12(2): 263-274 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Gulati B K, Sahu D, Sharma S, Vardhana Rao M V. Examining the Effect of Partial and Complete Elimination of a Specific Disease on the Gain in Life Expectancy at Birth in India and Selected States. JCHR 2023; 12 (2) :263-274
URL: http://jhr.ssu.ac.ir/article-1-773-en.html
URL: http://jhr.ssu.ac.ir/article-1-773-en.html
1- National Institute of Medical Statistics, Ansari Nagar, New Delhi, India , gulbk@hotmail.com
2- National Institute of Medical Statistics, Ansari Nagar, New Delhi, India
2- National Institute of Medical Statistics, Ansari Nagar, New Delhi, India
Full-Text [PDF 1270 kb]
(500 Downloads)
| Abstract (HTML) (1323 Views)
National Institute of Medical Statistics, Ansari Nagar, New Delhi, India

References
Full-Text: (272 Views)
| Examining the Effect of Partial and Complete Elimination of a Specific Disease on the Gain in Life Expectancy at Birth in India and Selected States |
National Institute of Medical Statistics, Ansari Nagar, New Delhi, India
| ARTICLE INFO | ABSTRACT | |
| Original Article Received: 08 Jun 2021 Accepted: 03 May 2023 |
Background: Life expectancy, especially life expectancy at birth, is a good indicator of current health condition of the population and is estimated through life tables. The present study aims to examine the effect of partial and complete elimination of a specific disease on the gain in life expectancy at birth by sex in India and selected states using Medical Certification of Cause of Death (MCCD) secondary data for 2017. Methods: Life tables were constructed for all cause-specific deaths using Greville method for both males and females separately for India and selected states. Cause-deleted life tables were also constructed for partial (25%, 50%, and 75%) and complete (100%) elimination of ten leading cause of death groups. Gain in life expectancy was estimated as the difference between values of cause-deleted life table and cause-specific life table. Results: Complete elimination of diseases of the circulatory system yielded maximum gain in life expectancy at birth in males (14.64 years) and in females (15.49 years) both in Haryana. It was followed by diseases of the respiratory system in males (6.45 years) in Jharkhand and in females (6.17 years) in Uttar Pradesh; certain infectious and parasitic diseases in males (3.82 years) in Uttar Pradesh and in females (3.58 years) in Delhi; neoplasms in males (2.71 years) and in females (2.11 years) both in Kerala. Similar results were obtained in case of remaining diseases. Conclusions: Maximum gained years in life expectancy at birth would be obtained after reducing or eliminating mortality from diseases of the circulatory system. These findings may help in setting up health goals, allocating resources, and launching tailor-made health care programmers. Keywords: Life Expectancy, MCCD, Non-Communicable Disease |
|
 |
||
Corresponding Author: Bal Kishan Gulati gulbk@hotmail.com |
How to cite this paper:
Gulati BK, Sahu D, Sharma S, Vardhana Rao M V. Examining the Effect of Partial and Complete Elimination of a Specific Disease on the Gain in Life Expectancy at Birth in India and Selected States. J Community Health Research 2023; 12(2): 263-274.
Introduction
Gulati BK, Sahu D, Sharma S, Vardhana Rao M V. Examining the Effect of Partial and Complete Elimination of a Specific Disease on the Gain in Life Expectancy at Birth in India and Selected States. J Community Health Research 2023; 12(2): 263-274.
Introduction
Life expectancy is a statistical measure to portray average life span a person is expected to live at a given age under given age-specific mortality rates and it is generated from life tables (1). A life table is an important demographic technique used in the analysis of mortality and other demographic processes (1). It is a succinct way of showing the probabilities of a member of a particular population living to or dying at a precise age (2). It presents a detailed sketch of a population that systematically gets depleted through death at each age.
As per Shkolnikov et al., period life expectancy is a measure of the average level of the hazard of death in a given calendar year and cohort life expectancy reflects the actual survival experiences of people born in a specific calendar year (3).
Glasen defined life expectancy at birth as the average number of years a new-born infant would live if prevailing patterns of mortality at the time of its birth were to stay the same throughout its life (4).
Crude death rate is not a precise indicator of mortality level or health condition in a country; therefore, life expectancy at birth is widely used in the analysis and description of level of mortality and it is a summary indicator to describe health and longevity of the population (5, 6).
Gain in life expectancy by eliminating a disease means that on average people will live more than they would in the presence of that disease. It represents the added years of life expectancy the population would receive if the deaths from a particular cause were reduced or eliminated as a competing risk of death (7- 10). It shows the effect of a certain disease on life expectancy, since it measures the reduction in life expectancy caused by the disease and provide a numerical indicator of survival if the disease is eliminated or reduced. In addition, this indicator is not affected by age structure of population, facilitating comparisons between diseases (11).
Life expectancy reflects the overall mortality level of a population and summarizes the mortality pattern that prevails across all age groups (children and adolescents, adults, and elderly) (12). It is the integrated survivorship of the population across all ages (13).
In mid-2000, women lived longer globally probably due to social and economic transformation benefitting women more than men (14). Urban life expectancy of female in India in 1970-75 (59.2 years) was slightly higher than in male (58.8 years) and the same trend is continuing till now. In 2014-18, the female life expectancy (73.8 years) is higher than that of male (71.5 years) by about two years (15).
Information on cause of death is important in mortality analysis and pattern of death by cause reveals the health status of the population and helps in making health plans. Though the medically certified cause of deaths from complete civil registration system is the ‘gold standard’ for such statistics, these are generally not available in a large number of countries (16).
Only a limited number of studies have been undertaken to estimate gain in life expectancy at birth using MCCD data. Therefore, the present study aimed to examine the effect of partial and complete elimination of a specific disease on the gain in life expectancy at birth in males and females in India and selected states by using MCCD data for the year 2017.
Methods
The principal data source used for analysis in this study is the annual Medical Certification of Cause of Death (MCCD) statistics report for 2017 which is available in public domain (17). The MCCD under Civil Registration System of India covers mostly those deaths, which occur in urban medical institutions. The necessary data was collected in the prescribed forms (form 4 for hospital deaths and form 4A for non-institutional deaths) which were attended to by the medical practitioners. These forms conformed to the international format of MCCD as evolved by the World Health Organization (WHO) comprising two parts incorporating immediate and antecedent causes of death along with identification and other details of the deceased. Part-I was used for entering the diseases in a specific sequence of events leading to death, so that immediate cause was recorded first and underlying cause, last. Part-II was used for recording the information on other significant morbid conditions, but not directly related to the cause of death (17). These forms were sent to Office of Registrar General of India (RGI) for tabulation and consolidation as per National List of Causes of Death based on Tenth Revision of International Classification of Disease (ICD-10) (18). More detailed information may be found elsewhere (19).
A study examined the consistency of the cause of death data and found that distribution of cause of deaths for the broad cause groups and top ten detailed causes was satisfactory (20).
All medically certified deaths occurred during 1st January to 31st December, 2017 in the hospitals covered under the scheme (whether public or private) mostly from urban areas and all non-institutional deaths which were attended to by the medical practitioners were included in the study. The MCCD-2017 report is based upon 14, 11, 060 total medically certified deaths [male: 8,73,368 (61.9%) and female: 5,37,692 (38.1%) with female to male sex ratio of 615 per thousand] accounting for 22.0 per cent of total registered deaths in respect of 35 States/UTs who supplied data for the report (17). The coverage of MCCD scheme and the percentage distribution of medically certified deaths of examined ten leading causes of deaths in India and selected states for 2017 are given in supplementary materials (Table 1). It may be seen that there was interstate variation in the coverage of MCCD scheme ranging from 4.7% in Jharkhand to 60.7% in Delhi (17).
Statistical analysis
In a life table, the term decrement refers to the mode of exiting the life table means death. (21). In a standard life table, sometimes referred to as a single decrement life table, ‘death’ is the only mode of exiting. In multiple-decrement life tables, more than one decrement operates and can be used to assess the contribution of different causes of death to the survival of the population (1, 21, 22). However, it cannot be used to assess the effect on life expectancy. To estimate the significance of a single cause of death, “cause-deleted” life tables need to be constructed (23). It is based on the assumption that mortality from all other causes of death would remain constant. The gain in life expectancy can be measured by comparing the life expectancy values of the cause-deleted life table with the life expectancy values of the standard (single decrement) life table.
The following steps were carried out to estimate gain in life expectancy through life table technique:
As per Shkolnikov et al., period life expectancy is a measure of the average level of the hazard of death in a given calendar year and cohort life expectancy reflects the actual survival experiences of people born in a specific calendar year (3).
Glasen defined life expectancy at birth as the average number of years a new-born infant would live if prevailing patterns of mortality at the time of its birth were to stay the same throughout its life (4).
Crude death rate is not a precise indicator of mortality level or health condition in a country; therefore, life expectancy at birth is widely used in the analysis and description of level of mortality and it is a summary indicator to describe health and longevity of the population (5, 6).
Gain in life expectancy by eliminating a disease means that on average people will live more than they would in the presence of that disease. It represents the added years of life expectancy the population would receive if the deaths from a particular cause were reduced or eliminated as a competing risk of death (7- 10). It shows the effect of a certain disease on life expectancy, since it measures the reduction in life expectancy caused by the disease and provide a numerical indicator of survival if the disease is eliminated or reduced. In addition, this indicator is not affected by age structure of population, facilitating comparisons between diseases (11).
Life expectancy reflects the overall mortality level of a population and summarizes the mortality pattern that prevails across all age groups (children and adolescents, adults, and elderly) (12). It is the integrated survivorship of the population across all ages (13).
In mid-2000, women lived longer globally probably due to social and economic transformation benefitting women more than men (14). Urban life expectancy of female in India in 1970-75 (59.2 years) was slightly higher than in male (58.8 years) and the same trend is continuing till now. In 2014-18, the female life expectancy (73.8 years) is higher than that of male (71.5 years) by about two years (15).
Information on cause of death is important in mortality analysis and pattern of death by cause reveals the health status of the population and helps in making health plans. Though the medically certified cause of deaths from complete civil registration system is the ‘gold standard’ for such statistics, these are generally not available in a large number of countries (16).
Only a limited number of studies have been undertaken to estimate gain in life expectancy at birth using MCCD data. Therefore, the present study aimed to examine the effect of partial and complete elimination of a specific disease on the gain in life expectancy at birth in males and females in India and selected states by using MCCD data for the year 2017.
Methods
The principal data source used for analysis in this study is the annual Medical Certification of Cause of Death (MCCD) statistics report for 2017 which is available in public domain (17). The MCCD under Civil Registration System of India covers mostly those deaths, which occur in urban medical institutions. The necessary data was collected in the prescribed forms (form 4 for hospital deaths and form 4A for non-institutional deaths) which were attended to by the medical practitioners. These forms conformed to the international format of MCCD as evolved by the World Health Organization (WHO) comprising two parts incorporating immediate and antecedent causes of death along with identification and other details of the deceased. Part-I was used for entering the diseases in a specific sequence of events leading to death, so that immediate cause was recorded first and underlying cause, last. Part-II was used for recording the information on other significant morbid conditions, but not directly related to the cause of death (17). These forms were sent to Office of Registrar General of India (RGI) for tabulation and consolidation as per National List of Causes of Death based on Tenth Revision of International Classification of Disease (ICD-10) (18). More detailed information may be found elsewhere (19).
A study examined the consistency of the cause of death data and found that distribution of cause of deaths for the broad cause groups and top ten detailed causes was satisfactory (20).
All medically certified deaths occurred during 1st January to 31st December, 2017 in the hospitals covered under the scheme (whether public or private) mostly from urban areas and all non-institutional deaths which were attended to by the medical practitioners were included in the study. The MCCD-2017 report is based upon 14, 11, 060 total medically certified deaths [male: 8,73,368 (61.9%) and female: 5,37,692 (38.1%) with female to male sex ratio of 615 per thousand] accounting for 22.0 per cent of total registered deaths in respect of 35 States/UTs who supplied data for the report (17). The coverage of MCCD scheme and the percentage distribution of medically certified deaths of examined ten leading causes of deaths in India and selected states for 2017 are given in supplementary materials (Table 1). It may be seen that there was interstate variation in the coverage of MCCD scheme ranging from 4.7% in Jharkhand to 60.7% in Delhi (17).
Statistical analysis
In a life table, the term decrement refers to the mode of exiting the life table means death. (21). In a standard life table, sometimes referred to as a single decrement life table, ‘death’ is the only mode of exiting. In multiple-decrement life tables, more than one decrement operates and can be used to assess the contribution of different causes of death to the survival of the population (1, 21, 22). However, it cannot be used to assess the effect on life expectancy. To estimate the significance of a single cause of death, “cause-deleted” life tables need to be constructed (23). It is based on the assumption that mortality from all other causes of death would remain constant. The gain in life expectancy can be measured by comparing the life expectancy values of the cause-deleted life table with the life expectancy values of the standard (single decrement) life table.
The following steps were carried out to estimate gain in life expectancy through life table technique:
- The initial deaths for leading cause of death groups were taken from the MCCD report for urban area 2017 (17). All the deaths in each cause of death group whose age was not stated was adjusted proportionately on the assumption that deaths with unreported age were in the same proportions in various age groups as those for which age was reported. Furthermore, these deaths were inflated to the estimated urban deaths based on the Sample Registration System (SRS) age specific death rates keeping the distribution of death by cause similar (24). An earlier study used this method for the estimation of cause-specific mortality in India (25). The base population for 2017 was obtained from the report of technical group on population projection (26). Crude birth rate and female to male sex ratio at birth for 2017 were taken from SRS (24). Abridged life tables were constructed according to the Greville method, which was incorporated into the spreadsheet calculation tool, using the cause of death (nmx) data for age groups < 1, 1-4, 5-14, 15-24, 25-34, 35-44, 45-54, 55-64, 65-69, and 70+ years for ten leading cause of death groups for males and females separately (27).
The nqx (the probability of dying between age x and x+n) values were estimated using the Greville formula (27):
.PNG)
Where, loge c = 0.09.
It is assumed that there is a linear relationship between age (x) and the natural log of the observed death rate (ln nmx) in accordance with the Gompertz law of mortality. A convenient approximation for C may be taken as loge c=0.09 though the values of loge c mostly vary between 0.080 and 0.104 (27). The remaining values were calculated as per usual notation of life table using spreadsheet.
2. Cause-deleted life tables (ex(-1)) were constructed for partial (25%, 50% and 75%) and complete (100%) elimination of deaths from the ten leading cause of death groups (Table 2 in supplementary materials).
3. Gain in life expectancy was estimated as the difference between life expectancy values of cause-deleted life table (ex(-1)) and life expectancy values of standard life table (ex) [(ex(-1)) − ex].
Results
The life tables were constructed for all cause-specific deaths for both males and females for India and selected states separately. The life tables were also constructed for cause-deleted partial (25%, 50%, and 75%) and complete (100%) elimination of ten leading cause of death groups. The life expectancy at birth (in years) considering all cause of death and life expectancy after complete elimination of ten leading cause of death groups are given in supplementary materials (Tables 3 and 4). Figures in bold in each column indicate the highest value in India and selected states. The calculated life expectancy at birth for India in 2017 is 73.4 years for males and 75.8 years for females compared to SRS life expectancy at birth of 71.5 years for males and 73.8 years for females in 2014-18. Among males, life expectancy at birth is the highest in West Bengal (75.6 years) and lowest in Chhattisgarh (67.6 years), compared to the highest in Delhi (80.8 years) and the lowest in Uttar Pradesh (71.1 years) among females.
Results highlighting the gain in life expectancy at birth in males and females for India and selected states after partial (25%, 50% and 75%) and complete (100%) elimination of mortality from ten leading cause of death groups are shown in supplementary materials (Tables 5-12). Figures in bold in each column indicate the highest value in India and selected states.
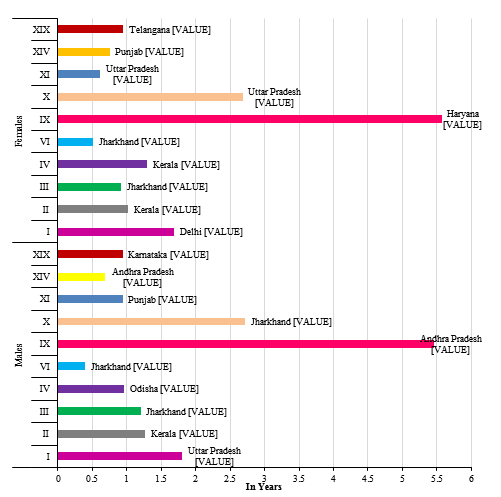
The results show that partial (25%) elimination of diseases of the circulatory system contributes the maximum gain in life expectancy at birth in males (2.43 years) in Andhra Pradesh and in females (2.45 years) in Haryana. It was followed by diseases of the respiratory system in males (1.26 years) in Jharkhand and in females (1.26 years) in Uttar Pradesh; certain infectious and parasitic diseases in males (0.87 years) in Uttar Pradesh and in females (0.82 years) in Delhi; and neoplasms in males (0.62 years) and in females (0.50 years) both in Kerala (Fig.1).
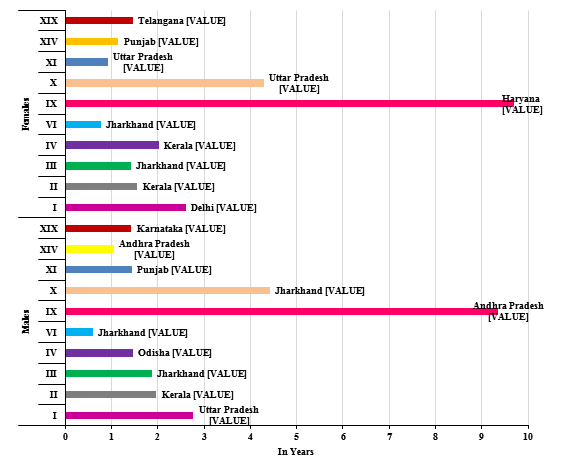
Partial (50%) elimination of diseases of the circulatory system leads to maximum gain in life expectancy at birth in males (5.46 years) in Andhra Pradesh and in females (5.57 years) in Haryana. It was followed by diseases of the respiratory system in males (2.72 years) in Jharkhand and in females (2.68 years) in Uttar Pradesh; certain infectious and parasitic diseases in males (1.80 years) in Uttar Pradesh and in females (1.69 years) in Delhi; and neoplasms in males (1.27 years) and in females (1.02 years) both in Kerala (Fig.2).
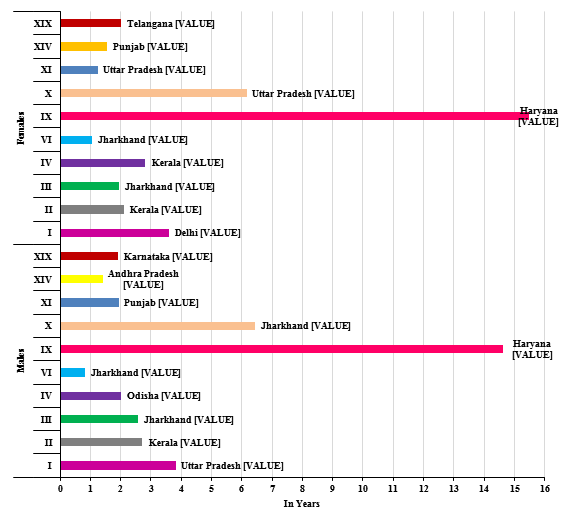
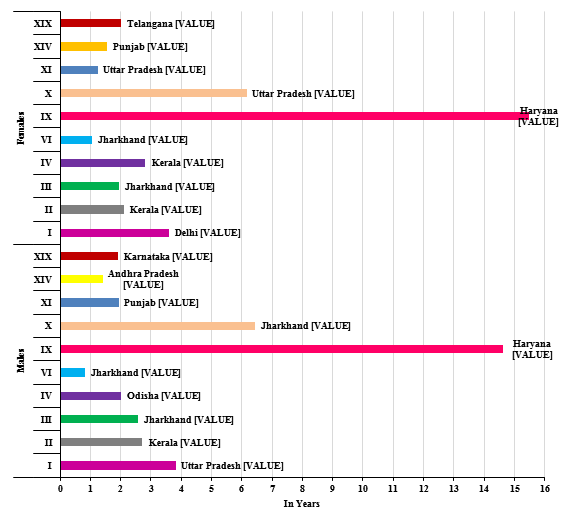
Partial (75%) elimination of diseases of the circulatory system leads to maximum gain in life expectancy at birth in males (9.36 years) in Andhra Pradesh and in females (9.69 years) in Haryana; followed by diseases of the respiratory system in males (4.42 years) in Jharkhand and in females (4.29 years) in Uttar Pradesh; certain infectious and parasitic diseases in males (2.77 years) in Uttar Pradesh and in females (2.61 years) in Delhi; and neoplasms in males (1.97 years) and in females (1.56 years) both in Kerala (Fig.3).
.PNG)
Where, loge c = 0.09.
It is assumed that there is a linear relationship between age (x) and the natural log of the observed death rate (ln nmx) in accordance with the Gompertz law of mortality. A convenient approximation for C may be taken as loge c=0.09 though the values of loge c mostly vary between 0.080 and 0.104 (27). The remaining values were calculated as per usual notation of life table using spreadsheet.
2. Cause-deleted life tables (ex(-1)) were constructed for partial (25%, 50% and 75%) and complete (100%) elimination of deaths from the ten leading cause of death groups (Table 2 in supplementary materials).
3. Gain in life expectancy was estimated as the difference between life expectancy values of cause-deleted life table (ex(-1)) and life expectancy values of standard life table (ex) [(ex(-1)) − ex].
Results
The life tables were constructed for all cause-specific deaths for both males and females for India and selected states separately. The life tables were also constructed for cause-deleted partial (25%, 50%, and 75%) and complete (100%) elimination of ten leading cause of death groups. The life expectancy at birth (in years) considering all cause of death and life expectancy after complete elimination of ten leading cause of death groups are given in supplementary materials (Tables 3 and 4). Figures in bold in each column indicate the highest value in India and selected states. The calculated life expectancy at birth for India in 2017 is 73.4 years for males and 75.8 years for females compared to SRS life expectancy at birth of 71.5 years for males and 73.8 years for females in 2014-18. Among males, life expectancy at birth is the highest in West Bengal (75.6 years) and lowest in Chhattisgarh (67.6 years), compared to the highest in Delhi (80.8 years) and the lowest in Uttar Pradesh (71.1 years) among females.
Results highlighting the gain in life expectancy at birth in males and females for India and selected states after partial (25%, 50% and 75%) and complete (100%) elimination of mortality from ten leading cause of death groups are shown in supplementary materials (Tables 5-12). Figures in bold in each column indicate the highest value in India and selected states.
The results show that partial (25%) elimination of diseases of the circulatory system contributes the maximum gain in life expectancy at birth in males (2.43 years) in Andhra Pradesh and in females (2.45 years) in Haryana. It was followed by diseases of the respiratory system in males (1.26 years) in Jharkhand and in females (1.26 years) in Uttar Pradesh; certain infectious and parasitic diseases in males (0.87 years) in Uttar Pradesh and in females (0.82 years) in Delhi; and neoplasms in males (0.62 years) and in females (0.50 years) both in Kerala (Fig.1).
Partial (50%) elimination of diseases of the circulatory system leads to maximum gain in life expectancy at birth in males (5.46 years) in Andhra Pradesh and in females (5.57 years) in Haryana. It was followed by diseases of the respiratory system in males (2.72 years) in Jharkhand and in females (2.68 years) in Uttar Pradesh; certain infectious and parasitic diseases in males (1.80 years) in Uttar Pradesh and in females (1.69 years) in Delhi; and neoplasms in males (1.27 years) and in females (1.02 years) both in Kerala (Fig.2).
Partial (75%) elimination of diseases of the circulatory system leads to maximum gain in life expectancy at birth in males (9.36 years) in Andhra Pradesh and in females (9.69 years) in Haryana; followed by diseases of the respiratory system in males (4.42 years) in Jharkhand and in females (4.29 years) in Uttar Pradesh; certain infectious and parasitic diseases in males (2.77 years) in Uttar Pradesh and in females (2.61 years) in Delhi; and neoplasms in males (1.97 years) and in females (1.56 years) both in Kerala (Fig.3).

Figure 1. Gain in life expectancy at birth (in years) in males and females after partial (25%) elimination of specific cause of death, India and selected states (MCCD, 2017)
|
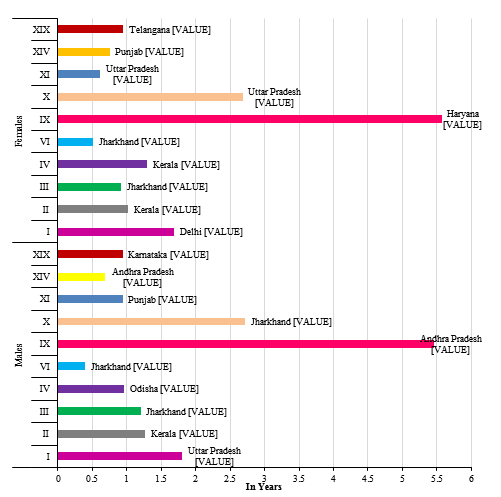
Figure 2. Gain in life expectancy at birth (in years) in males and females after partial (50%) elimination of specific cause of death, India and selected states (MCCD, 2017)
|
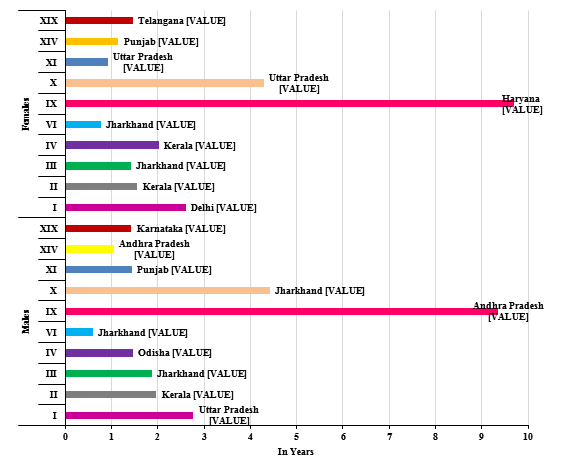
Figure 3. Gain in life expectancy at birth (in years) in males and females after partial (75%) elimination of specific cause of death, India and selected states (MCCD, 2017)
|
|
Figure 4. Gain in life expectancy at birth (in years) in males and females after complete (100%) elimination of specific cause of death, India and selected states (MCCD, 2017)
Complete (100%) elimination of diseases of the circulatory system leads to maximum gain in life expectancy at birth in males (14.64 years) and in females (15.49 years) both in Haryana (Fig.4). It was followed by diseases of the respiratory system in males (6.45 years) in Jharkhand and in females (6.17 years) in Uttar Pradesh; certain infectious and parasitic diseases in males (3.82 years) in Uttar Pradesh and in females (3.58 years) in Delhi; neoplasms in males (2.71 years) and in females (2.11 years) both in Kerala; diseases of blood and blood forming organs and certain disorders involving the immune mechanism in males (2.58 years) and in females (1.94 years) both in Jharkhand (Fig.4). It was followed by endocrine, nutritional and metabolic diseases in males (2.02 years) in Odisha and in females (2.81 years) in Kerala; diseases of the digestive system in males (1.95 years) in Punjab and in females (1.25 years) in Uttar Pradesh; injury, poisoning and certain other consequences of external causes in males (1.91 years) in Karnataka and in females (2.02 years) in Telangana (Fig.4). It was followed by diseases of the genitourinary system in males (1.42 years) in Andhra Pradesh and in females (1.56 years) in Punjab; and diseases of the nervous system in males (0.81 years) and in females (1.06 years) both in Jharkhand (Fig.4).
It is worthy to note that partial as well as complete elimination of the diseases of the circulatory diseases leads to maximum gain in life expectancy at birth in males and females in India and selected states.
Discussion
In this study, it was found that complete elimination of diseases of the circulatory system yielded the maximum gain in life expectancy at birth in males (14.64 years) and in females (15.49 years) both in Haryana. It was followed by diseases of the respiratory system in males (6.45 years) in Jharkhand and in females (6.17 years) in Uttar Pradesh; certain infectious and parasitic diseases in males (3.82 years) in Uttar Pradesh and in females (3.58 years) in Delhi; neoplasms in males (2.71 years) and in females (2.11 years) both in Kerala; diseases of blood and blood forming organs and certain disorders involving the immune mechanism in males (2.58 years) and in females (1.94 years) both in Jharkhand. It was followed by endocrine, nutritional and metabolic diseases in males (2.02 years) in Odisha and in females (2.81 years) in Kerala; diseases of the digestive system in males (1.95 years) in Punjab and in females (1.25 years) in Uttar Pradesh; injury, poisoning and certain other consequences of external causes in males (1.91 years) in Karnataka and in females (2.02 years) in Telangana. It was followed by diseases of the genitourinary system in males (1.42 years) in Andhra Pradesh and in females (1.56 years) in Punjab; and diseases of the nervous system in males (0.81 years) and in females (1.06 years) both in Jharkhand.
It is clear that both males and females are more burdened with diseases of the circulatory system; diseases of the respiratory system; certain infectious and parasitic diseases; and neoplasms in India and 18 selected states. Partial and complete elimination of these diseases would provide the maximum gain in life expectancy at birth. The study findings are in line with findings of other similar studies. Tsai et al. (28) found that complete elimination of cardiovascular disease would add 11.10 and 12.81 years in life expectancy at birth for white males and females, respectively. In case of non-white males and females, it would add 10.74 and 15.66 years, respectively, in the USA. Jayachandran (29) found that the maximum gain in life expectancy at birth for males (3.49 years) was from respiratory disorders (cough) eliminated cause and for females the cause was fever (3.21 years). Kulkarni et al. (30) found that net gain in life expectancy at birth was 11.5 and 15.2 years in males and females, respectively when mortality due to cardiovascular diseases was eliminated in Goa. A similar study found that net gain in life expectancy at birth was 9.4 years in males and 11.3 years in females in India; 10.0/11.8 years in Maharashtra; and 7.6/11.6 years in Rajasthan after complete elimination of the diseases of the circulatory system (19). Another similar study highlighted the net gain in life expectancy at birth after complete elimination of mortality from diseases of the circulatory system (11.1 years in males and 13.1 years in females). It was followed by certain infectious and parasitic diseases (2.2/2.1 years); diseases of the respiratory system (2.2/2.1 years); injury, poisoning and certain other consequences of external causes (1.1/0.7 years); neoplasms (0.9/1.0 years).It was followed by endocrine, nutritional, and metabolic diseases (0.8/0.9 years); diseases of the digestive system (0.8/0.4 years); diseases of the genitourinary system (0.6/0.6 years); diseases of the nervous system (0.4/0.4 years); and diseases of blood and blood forming organs and certain disorders involving the immune mechanism (0.2/0.3 years) (31).
This study highlights the effect of each cause of death on life expectancy at birth in India and selected states. The pattern of death by cause shows the health status of the study population and would be helpful in making health plans. It may also help planner and policy makers to take appropriate intervention measures to reduce mortality levels. The study results showed that diseases of the circulatory system are the largest contributor to disease burden and are a major public health problem leading to premature deaths and morbidity across all selected states of India which is on the same lines of findings of an earlier study (32). This needs to be addressed urgently by each state by adopting preventive and management strategies according to the magnitude of its burden. The policymakers should revamp the existing public health facilities and strengthen it by setting up primary and community health centers, and other governments’ health facilities in India.
In 2010, the Govt. of India launched the National Program for Prevention and Control of Cancer, Diabetes, Cardiovascular Diseases and Stroke (NPCDCS) with the objectives to prevent and control disease burden by strengthening infrastructure, human resource development, health promotion, early diagnosis, management and referral (33). Till March 2017, non-communicable diseases (NCD) units were established in all states and :union: territories. However, implementation of these and other efforts needs some more time to show progress made towards achieving national and global targets for non-communicable diseases, including cardiovascular diseases. In early 2018, India has implemented the Ayushman Bharat, the National Health Protection Mission, with the main purpose of improving the primary health centers/community health centers into health and wellness centers with better and improved healthcare facilities, and provision of insurance of Rs.5.00 lakhs for each household below the poverty line for their treatment as increasing burden of diseases places further economic pressure on individuals and households (34, 35).
It is pertinent to note that six causes of death groups viz, diseases of the circulatory system (34%), certain infectious and parasitic diseases (10.4%), diseases of the respiratory system (9.2%), neoplasms (6.4%), injury, poisoning and certain other consequences of external causes (5.8%) and diseases of the digestive system (4.4%) constituted around 70% of the total medically certified deaths in the year 2017. In the total registered deaths of 6426595 in India in 2017, there were 1183052 medically certified (urban) deaths (22%) (17). As per census 2011, around 70% (68.84%) population lives in rural areas (36) and if we take into consideration the same percentage of the total medically certified deaths and calculate the number of deaths under these six leading cause of death groups, we would have a substantial number of deaths in rural areas to be averted after eliminating these diseases.
Conclusion
As per study findings, maximum gained years in life expectancy at birth would be obtained after reducing or eliminating mortality from diseases of the circulatory system by implementing intervention programmes and by making changes in lifestyle with focus on both behavioral and dietary habits. These findings may help in setting up health goals, allocating resources and launching tailor-made health care programmess.
Strengths and Limitations of the study
The burden of diseases, as measured by the study findings may help to identify suitable population goals for interventions for disease reduction in India. Although the study has several strengths, it has some limitations as well. We did not calculate the quality of health care, life style, economy, environment etc., and life expectancy is affected by these factors. Hypothesis of complete elimination of certain diseases that cause death is not realistic. Improvement in the coverage of MCCD scheme is required for further strengthening of the study findings.
Acknowledgement
The authors are grateful to DG, ICMR for confirming the research project entitled “Gain in life expectancy by age after elimination of death due to specific cause in selected states of India using MCCD data”, results of which are summarized in this paper. Technical help rendered by Shri Ganesh Prasad Jena is also acknowledged. This study used secondary data accessible from a national descriptive tabulation report and use of such aggregate data does not require ethical approval.
Conflict of interest
None declared.
Funding
None declared.
Ethical considerations
None declared. Used secondary data available in public domain.
Code of Ethics
Implemented
Authors’ contribution
BKG and DS designed the study; BKG analyzed the data and wrote the manuscript; DS, SS and MVVR critically edited the manuscript.
Open Access Policy
JCHR does not charge readers and their institution for access to its papers. Full text download of all new and archived papers are free of charge.
It is worthy to note that partial as well as complete elimination of the diseases of the circulatory diseases leads to maximum gain in life expectancy at birth in males and females in India and selected states.
Discussion
In this study, it was found that complete elimination of diseases of the circulatory system yielded the maximum gain in life expectancy at birth in males (14.64 years) and in females (15.49 years) both in Haryana. It was followed by diseases of the respiratory system in males (6.45 years) in Jharkhand and in females (6.17 years) in Uttar Pradesh; certain infectious and parasitic diseases in males (3.82 years) in Uttar Pradesh and in females (3.58 years) in Delhi; neoplasms in males (2.71 years) and in females (2.11 years) both in Kerala; diseases of blood and blood forming organs and certain disorders involving the immune mechanism in males (2.58 years) and in females (1.94 years) both in Jharkhand. It was followed by endocrine, nutritional and metabolic diseases in males (2.02 years) in Odisha and in females (2.81 years) in Kerala; diseases of the digestive system in males (1.95 years) in Punjab and in females (1.25 years) in Uttar Pradesh; injury, poisoning and certain other consequences of external causes in males (1.91 years) in Karnataka and in females (2.02 years) in Telangana. It was followed by diseases of the genitourinary system in males (1.42 years) in Andhra Pradesh and in females (1.56 years) in Punjab; and diseases of the nervous system in males (0.81 years) and in females (1.06 years) both in Jharkhand.
It is clear that both males and females are more burdened with diseases of the circulatory system; diseases of the respiratory system; certain infectious and parasitic diseases; and neoplasms in India and 18 selected states. Partial and complete elimination of these diseases would provide the maximum gain in life expectancy at birth. The study findings are in line with findings of other similar studies. Tsai et al. (28) found that complete elimination of cardiovascular disease would add 11.10 and 12.81 years in life expectancy at birth for white males and females, respectively. In case of non-white males and females, it would add 10.74 and 15.66 years, respectively, in the USA. Jayachandran (29) found that the maximum gain in life expectancy at birth for males (3.49 years) was from respiratory disorders (cough) eliminated cause and for females the cause was fever (3.21 years). Kulkarni et al. (30) found that net gain in life expectancy at birth was 11.5 and 15.2 years in males and females, respectively when mortality due to cardiovascular diseases was eliminated in Goa. A similar study found that net gain in life expectancy at birth was 9.4 years in males and 11.3 years in females in India; 10.0/11.8 years in Maharashtra; and 7.6/11.6 years in Rajasthan after complete elimination of the diseases of the circulatory system (19). Another similar study highlighted the net gain in life expectancy at birth after complete elimination of mortality from diseases of the circulatory system (11.1 years in males and 13.1 years in females). It was followed by certain infectious and parasitic diseases (2.2/2.1 years); diseases of the respiratory system (2.2/2.1 years); injury, poisoning and certain other consequences of external causes (1.1/0.7 years); neoplasms (0.9/1.0 years).It was followed by endocrine, nutritional, and metabolic diseases (0.8/0.9 years); diseases of the digestive system (0.8/0.4 years); diseases of the genitourinary system (0.6/0.6 years); diseases of the nervous system (0.4/0.4 years); and diseases of blood and blood forming organs and certain disorders involving the immune mechanism (0.2/0.3 years) (31).
This study highlights the effect of each cause of death on life expectancy at birth in India and selected states. The pattern of death by cause shows the health status of the study population and would be helpful in making health plans. It may also help planner and policy makers to take appropriate intervention measures to reduce mortality levels. The study results showed that diseases of the circulatory system are the largest contributor to disease burden and are a major public health problem leading to premature deaths and morbidity across all selected states of India which is on the same lines of findings of an earlier study (32). This needs to be addressed urgently by each state by adopting preventive and management strategies according to the magnitude of its burden. The policymakers should revamp the existing public health facilities and strengthen it by setting up primary and community health centers, and other governments’ health facilities in India.
In 2010, the Govt. of India launched the National Program for Prevention and Control of Cancer, Diabetes, Cardiovascular Diseases and Stroke (NPCDCS) with the objectives to prevent and control disease burden by strengthening infrastructure, human resource development, health promotion, early diagnosis, management and referral (33). Till March 2017, non-communicable diseases (NCD) units were established in all states and :union: territories. However, implementation of these and other efforts needs some more time to show progress made towards achieving national and global targets for non-communicable diseases, including cardiovascular diseases. In early 2018, India has implemented the Ayushman Bharat, the National Health Protection Mission, with the main purpose of improving the primary health centers/community health centers into health and wellness centers with better and improved healthcare facilities, and provision of insurance of Rs.5.00 lakhs for each household below the poverty line for their treatment as increasing burden of diseases places further economic pressure on individuals and households (34, 35).
It is pertinent to note that six causes of death groups viz, diseases of the circulatory system (34%), certain infectious and parasitic diseases (10.4%), diseases of the respiratory system (9.2%), neoplasms (6.4%), injury, poisoning and certain other consequences of external causes (5.8%) and diseases of the digestive system (4.4%) constituted around 70% of the total medically certified deaths in the year 2017. In the total registered deaths of 6426595 in India in 2017, there were 1183052 medically certified (urban) deaths (22%) (17). As per census 2011, around 70% (68.84%) population lives in rural areas (36) and if we take into consideration the same percentage of the total medically certified deaths and calculate the number of deaths under these six leading cause of death groups, we would have a substantial number of deaths in rural areas to be averted after eliminating these diseases.
Conclusion
As per study findings, maximum gained years in life expectancy at birth would be obtained after reducing or eliminating mortality from diseases of the circulatory system by implementing intervention programmes and by making changes in lifestyle with focus on both behavioral and dietary habits. These findings may help in setting up health goals, allocating resources and launching tailor-made health care programmess.
Strengths and Limitations of the study
The burden of diseases, as measured by the study findings may help to identify suitable population goals for interventions for disease reduction in India. Although the study has several strengths, it has some limitations as well. We did not calculate the quality of health care, life style, economy, environment etc., and life expectancy is affected by these factors. Hypothesis of complete elimination of certain diseases that cause death is not realistic. Improvement in the coverage of MCCD scheme is required for further strengthening of the study findings.
Acknowledgement
The authors are grateful to DG, ICMR for confirming the research project entitled “Gain in life expectancy by age after elimination of death due to specific cause in selected states of India using MCCD data”, results of which are summarized in this paper. Technical help rendered by Shri Ganesh Prasad Jena is also acknowledged. This study used secondary data accessible from a national descriptive tabulation report and use of such aggregate data does not require ethical approval.
Conflict of interest
None declared.
Funding
None declared.
Ethical considerations
None declared. Used secondary data available in public domain.
Code of Ethics
Implemented
Authors’ contribution
BKG and DS designed the study; BKG analyzed the data and wrote the manuscript; DS, SS and MVVR critically edited the manuscript.
Open Access Policy
JCHR does not charge readers and their institution for access to its papers. Full text download of all new and archived papers are free of charge.
References
- Preston SH, Heuveline P, et al. Demography: Measuring and Modeling Population Processes. Malden, MA, Blackwell Publishing. 2001.
- Jose MP, Francisco M, Josep L. Introducing migratory flows in life table construction. SORT. 2012; 36(1): 103-114.
- Shkolnikov VM, Jdanov DA, Andreev EM, et al. Steep increase in best-practice cohort life expectancy. Population and Development Review. 2011; 37(3): 419-434.
- Glasen P. Basic antecedents of life expectancy at birth. Linear regression modelling. Munich: GRIN Verlag. 2015. Available at: URL: https://www.grin.com/document/311417.
5. Rabbi Fazle AM. Imbalance in life table: Effect of infant mortality on lower life expectancy at birth. Journal of Scientific Research. 2013; 5(3): 479-488. https://doi.org/10.3329/jsr.v5i3.14105.
6. Sharma R. Health and economic growth: Evidence from dynamic panel data of 143 years. PLoS ONE. 2018; 13(10): e0204940. https://doi.org/10.1371/journal.pone.0204940.
7. Conti S, Farchi G, Masocco M, et al. The impact of the major causes of death on life expectancy in Italy. International Journal of Epidemiology. 1999; 28(5): 905-910.
8. Lai D, Hardy RJ. Potential gains in life expectancy or years of potential life lost: impact of competing risks of death. International Journal of Epidemiology. 1999; 28: 894-898.
9. Wang HG. Study on the Influence of Main Diseases to Life expectancy of Chinese Residents. Peking :union: Medical College, Master Thesis; 2011.
10. Elizabeth A, Melonie H, Betzaida T. United States life tables eliminating certain causes of death, 1999–2001. National Vital Statistics Report. 2013; 9(61): 1-128.
11. Zhao NQ, Chen F. Health Statistics. Beijing: Higher Education Press; 2008.
12. World Health Organization. World Health Statistics 2014. Geneva: WHO; 2014.
13. Missov TI. Gamma-Gompertz life expectancy at birth. Demographic Research. 2013; 28(9): 259–270. https://doi.org/10.4054/DemRes.2012.28.9.
14. Barford A, Dorling D, Smith GD, et al. Life expectancy: women now on top everywhere. Bmj. 2006; 332(7545): 808.
15. Registrar General of India. SRS Based Abridged Life Tables 2014-18. Ministry of Home Affairs, Government of India; 2020.
16. Mathers CD, Fat DM, Inoue M, et al. Counting the death and what they died from: an assessment of the global status of cause of death data. Bulletin of the World Health Organization. 2005; 83(3): 172-177.
17. Registrar General of India. Report on Medical Certification of Cause of Death, 2017. Ministry of Home Affairs, Vital Statistics Division, Government of India; 2019.
18. World Health Organization. International statistical classification of diseases and related health problems, tenth revision. Geneva: WHO Press; 1993.
19. Gulati BK, Pandey A, Ubaidullah M. Potential gain in life expectancy after partial and complete elimination of specified causes of death: An analysis of Medical Certification of Causes of Death data in India and its selected states; International Journal of Multidisciplinary Research and Development. 2015; 2(4): 508-512.
20. Mahapatra P & Rao CPV. Cause of death reporting systems in India: A performance analysis. National Medical Journal of India. 2001; 14(3): 154-162.
21. Hinde A. Demographic Methods. London: Arnold publishers; 1998.
22. Siegel JS and Swanson DA. (Editors). The Methods and Materials of Demography, 2nd Edition. London: Elsevier Academic Press; 2004.
23. Beltran-Sanchez H, Preston SH, Canudas-Romo V. An integrated approach to cause-of-death analysis: cause-deleted life tables and decompositions of life expectancy. Demographic Research. 2008; 19 (35): 1323–1350. doi: 10.4054/DemRes.
24. Registrar General of India. Sample Registration System Statistical Report 2017. Ministry of Home Affairs, Government of India; 2018.
25. Murray CJL & Lopez A. The global burden of disease: A comprehensive assessment of mortality and diseases, injuries, and risk factors in 1990 and projected to 2020. Global Burden of Disease and Injury Series, 1. Cambridge, MA: Harvard University Press, Harvard School of Public Health. 1996.
26. Registrar General of India. Population Projection for India and States 2011–2036. Report of the Technical Group on Population Projections. Ministry of Home Affairs, Government of India; 2020.
27. Greville TNE. Short methods of constructing abridged life tables. Record of the American Institute of Actuaries. 1943; 32(65): 29-42.
28. Tsai SP, Lee ES, Hardy RJ. The Effect of a Reduction in Leading causes of Death: Potential Gains in Life Expectancy. American Journal of Public Health. 1978; 68(10): 966-971.
29. Jayachandran V. Study of cause of death and differential life expectancies in India: An empirical approach. Ph.D. Thesis, International Institute for Population Sciences, Mumbai; 1999.
30. Kulkarni MS, Ferreira AMA, Motghare DD. Potential gain in life expectancy with control of cardiovascular disease in India: A case study from Goa state. South Asian Journal of Preventive Oncology. 2004; 8(4).
31. Gulati BK, Sahu D, Kumar A, et al. Potential gain in life expectancy by gender after elimination of a specific cause of death in urban India. International Journal of Community Medicine and Public Health. 2020; 7(5): 1848-53.
32. GBD 2016 India State-Level Disease Burden Initiative CVD Collaborators. The changing patterns of cardiovascular diseases and their risk factors in the states of India: the Global Burden of Disease Study 1990-2016. Lancet Glob Health. 2018; 6: e1339-51.
33. http://dghs.gov.in (accessed May 28, 2021).
34. http://pmjay.gov.in (accessed May 28, 2021).
35. Jan S, Laba T-L, Essue BM, et al. Action to address the household economic burden of non-communicable diseases. Lancet. 2018; 391: 2047-58.
36. Registrar General of India. Provisional Population Totals: India. Census of India, Ministry of Home Affairs, Government of India; 2011.
6. Sharma R. Health and economic growth: Evidence from dynamic panel data of 143 years. PLoS ONE. 2018; 13(10): e0204940. https://doi.org/10.1371/journal.pone.0204940.
7. Conti S, Farchi G, Masocco M, et al. The impact of the major causes of death on life expectancy in Italy. International Journal of Epidemiology. 1999; 28(5): 905-910.
8. Lai D, Hardy RJ. Potential gains in life expectancy or years of potential life lost: impact of competing risks of death. International Journal of Epidemiology. 1999; 28: 894-898.
9. Wang HG. Study on the Influence of Main Diseases to Life expectancy of Chinese Residents. Peking :union: Medical College, Master Thesis; 2011.
10. Elizabeth A, Melonie H, Betzaida T. United States life tables eliminating certain causes of death, 1999–2001. National Vital Statistics Report. 2013; 9(61): 1-128.
11. Zhao NQ, Chen F. Health Statistics. Beijing: Higher Education Press; 2008.
12. World Health Organization. World Health Statistics 2014. Geneva: WHO; 2014.
13. Missov TI. Gamma-Gompertz life expectancy at birth. Demographic Research. 2013; 28(9): 259–270. https://doi.org/10.4054/DemRes.2012.28.9.
14. Barford A, Dorling D, Smith GD, et al. Life expectancy: women now on top everywhere. Bmj. 2006; 332(7545): 808.
15. Registrar General of India. SRS Based Abridged Life Tables 2014-18. Ministry of Home Affairs, Government of India; 2020.
16. Mathers CD, Fat DM, Inoue M, et al. Counting the death and what they died from: an assessment of the global status of cause of death data. Bulletin of the World Health Organization. 2005; 83(3): 172-177.
17. Registrar General of India. Report on Medical Certification of Cause of Death, 2017. Ministry of Home Affairs, Vital Statistics Division, Government of India; 2019.
18. World Health Organization. International statistical classification of diseases and related health problems, tenth revision. Geneva: WHO Press; 1993.
19. Gulati BK, Pandey A, Ubaidullah M. Potential gain in life expectancy after partial and complete elimination of specified causes of death: An analysis of Medical Certification of Causes of Death data in India and its selected states; International Journal of Multidisciplinary Research and Development. 2015; 2(4): 508-512.
20. Mahapatra P & Rao CPV. Cause of death reporting systems in India: A performance analysis. National Medical Journal of India. 2001; 14(3): 154-162.
21. Hinde A. Demographic Methods. London: Arnold publishers; 1998.
22. Siegel JS and Swanson DA. (Editors). The Methods and Materials of Demography, 2nd Edition. London: Elsevier Academic Press; 2004.
23. Beltran-Sanchez H, Preston SH, Canudas-Romo V. An integrated approach to cause-of-death analysis: cause-deleted life tables and decompositions of life expectancy. Demographic Research. 2008; 19 (35): 1323–1350. doi: 10.4054/DemRes.
24. Registrar General of India. Sample Registration System Statistical Report 2017. Ministry of Home Affairs, Government of India; 2018.
25. Murray CJL & Lopez A. The global burden of disease: A comprehensive assessment of mortality and diseases, injuries, and risk factors in 1990 and projected to 2020. Global Burden of Disease and Injury Series, 1. Cambridge, MA: Harvard University Press, Harvard School of Public Health. 1996.
26. Registrar General of India. Population Projection for India and States 2011–2036. Report of the Technical Group on Population Projections. Ministry of Home Affairs, Government of India; 2020.
27. Greville TNE. Short methods of constructing abridged life tables. Record of the American Institute of Actuaries. 1943; 32(65): 29-42.
28. Tsai SP, Lee ES, Hardy RJ. The Effect of a Reduction in Leading causes of Death: Potential Gains in Life Expectancy. American Journal of Public Health. 1978; 68(10): 966-971.
29. Jayachandran V. Study of cause of death and differential life expectancies in India: An empirical approach. Ph.D. Thesis, International Institute for Population Sciences, Mumbai; 1999.
30. Kulkarni MS, Ferreira AMA, Motghare DD. Potential gain in life expectancy with control of cardiovascular disease in India: A case study from Goa state. South Asian Journal of Preventive Oncology. 2004; 8(4).
31. Gulati BK, Sahu D, Kumar A, et al. Potential gain in life expectancy by gender after elimination of a specific cause of death in urban India. International Journal of Community Medicine and Public Health. 2020; 7(5): 1848-53.
32. GBD 2016 India State-Level Disease Burden Initiative CVD Collaborators. The changing patterns of cardiovascular diseases and their risk factors in the states of India: the Global Burden of Disease Study 1990-2016. Lancet Glob Health. 2018; 6: e1339-51.
33. http://dghs.gov.in (accessed May 28, 2021).
34. http://pmjay.gov.in (accessed May 28, 2021).
35. Jan S, Laba T-L, Essue BM, et al. Action to address the household economic burden of non-communicable diseases. Lancet. 2018; 391: 2047-58.
36. Registrar General of India. Provisional Population Totals: India. Census of India, Ministry of Home Affairs, Government of India; 2011.
Review: Research |
Subject:
Public Health
Received: 2023/02/8 | Accepted: 2023/05/3 | Published: 2023/11/28
Received: 2023/02/8 | Accepted: 2023/05/3 | Published: 2023/11/28
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution 4.0 International License. |