Volume 12, Issue 1 (3-2023)
JCHR 2023, 12(1): 7-17 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Ziaadini M, Abolhasani M S, Khazaee H, Zarezadeh M, Asadi S, Ghorbani F et al . Explaining the Factors Involved in Psychological Effects of Covid-19 on Health Care Workers by Interpretive Structural Modeling. JCHR 2023; 12 (1) :7-17
URL: http://jhr.ssu.ac.ir/article-1-733-en.html
URL: http://jhr.ssu.ac.ir/article-1-733-en.html
Mohammad Ziaadini1 

 , Mohammad Sadegh Abolhasani *
, Mohammad Sadegh Abolhasani * 

 2, Homa Khazaee3
2, Homa Khazaee3 

 , Mohammad Zarezadeh3
, Mohammad Zarezadeh3 

 , Sedigheh Asadi3
, Sedigheh Asadi3 

 , Farzaneh Ghorbani3
, Farzaneh Ghorbani3 

 , Elaheh Salarikhah3
, Elaheh Salarikhah3 




 , Mohammad Sadegh Abolhasani *
, Mohammad Sadegh Abolhasani * 

 2, Homa Khazaee3
2, Homa Khazaee3 

 , Mohammad Zarezadeh3
, Mohammad Zarezadeh3 

 , Sedigheh Asadi3
, Sedigheh Asadi3 

 , Farzaneh Ghorbani3
, Farzaneh Ghorbani3 

 , Elaheh Salarikhah3
, Elaheh Salarikhah3 


1- Department of Management, Rafsanjan Branch, Islamic Azad University, Rafsanjan, Iran
2- Department of Management, Rafsanjan Branch, Islamic Azad University, Rafsanjan, Iran , Mziaaddini@yahoo.com
3- ShahidSadoughi University of Medical Sciences Yazd, Yazd, Iran
2- Department of Management, Rafsanjan Branch, Islamic Azad University, Rafsanjan, Iran , Mziaaddini@yahoo.com
3- ShahidSadoughi University of Medical Sciences Yazd, Yazd, Iran
Full-Text [PDF 302 kb]
(356 Downloads)
| Abstract (HTML) (587 Views)
How to cite this paper:
Introduction
A: If i affects j and j affects i, too.
X: If only j affects i.
O: If there is no relationship between i and j.
According to Warfield instruction (1974) (13), the experts’ opinions were used to determine the relationship between the obstacles to tourism development.
Initial reachability matrix
The structural self-interaction matrix changes into a zero-one matrix that is called the initial reachability matrix. This matrix only includes zero and one. Replacement of zero and one for the four primary numbers (0, -1, 1, and 2) is done as the following:
If the intersection of i and j in SSIM is equal to V, in the reachability matrix (i, j) will be equal to 1 and (j, i) will be equal to 0.
If the intersection of (i, j) in SSIM is equal to A, in the reachability matrix both (i, j) and (j, i) will be equal to 1.
If the intersection of (i, j) in SSIM is equal to X, in the reachability matrix both (i, j) and (j, i) will be equal to 0.
If the intersection of (i, j) in SSIM is equal to O, in the reachability matrix (i, j) will be equal to 0 and (j, i) will be equal to 1.
In matrix D i.e. the initial reachability matrix, zero and one are replaced for each of the dij indicators, while cj indicates the factors involved in reduction of the mental pressure imposed by coronavirus conditions.
Final reachability matrix
M*=MK=MK+1R c j ∩ A c j R c j ∀ c j ∈ C
Clustering the criteria
To show the one-way effect (criterion i leads to criterion j) V
To show a one-way effect (criterion j leads to criterion i) A
To show the two-way influence of X
To show the lack of relationship between the two criteria O
Table 3. Primary access matrix Factors affecting the psychological effects of Covid-19

References
1. Shigemura J, Ursano RJ, Morganstein JC, Kurosawa M, Benedek DM. Public responses to the novel 2019 coronavirus (2019‐nCoV) in Japan: Mental health consequences and target populations. Psychiatry and clinical neurosciences. 2020; 74(4): 281.
2. Zhang F, Shang Z, Ma H, Jia Y, Sun L, et al. High risk of infection caused posttraumatic stress symptoms in individuals with poor sleep quality: A study on influence of coronavirus disease (COVID-19) in China. MedRxiv. 2020.
3. Lai C-C, Shih T-P, Ko W-C, Tang H-J, Hsueh P-R. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease-2019 (COVID-19): The epidemic and the challenges. International journal of antimicrobial agents. 2020; 55(3): 105924.
4. Li S, Wang Y, Xue J, Zhao N, Zhu T. The impact of COVID-19 epidemic declaration on psychological consequences: a study on active Weibo users. International journal of environmental research and public health. 2020; 17(6): 2032.
5. Bao Y, Sun Y, Meng S, Shi J, Lu L. 2019-nCoV epidemic: address mental health care to empower society. The Lancet. 2020; 395(10224): e37-e8.
6. Chen Q, Liang M, Li Y, Guo J, Fei D, et al. Mental health care for medical staff in China during the COVID-19 outbreak. The Lancet Psychiatry. 2020; 7(4): e15-e6.
7. Xiang Y-T, Yang Y, Li W, Zhang L, Zhang Q, et al. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. The lancet psychiatry. 2020; 7(3): 228-9.
8. Kittrell Chitty K. Professional nursing concepts & challenges. Amsterdam, Netherlands: Elsevier Science Health Science div; 2004.
9. Perry AG, Potter P. Basic nursing: Essentials for practice: Mosby, Elsevier; 2003.
10. Kang L, Li Y, Hu S, Chen M, Yang C, et al. The mental health of medical workers in Wuhan, China dealing with the 2019 novel coronavirus. The Lancet Psychiatry. 2020.
11. Li L, Wan C, Ding R, Liu Y, Chen J, et al. Mental distress among Liberian medical staff working at the China Ebola Treatment Unit: a cross sectional study. Health and quality of life outcomes. 2015; 13(1): 1-6.
12. Huang L, rong Liu H. Emotional responses and coping strategies of nurses and nursing college students during COVID-19 outbreak. MedRxiv. 2020.
13. Warfield JN. Developing interconnection matrices in structural modeling. IEEE Transactions on Systems, Man, and Cybernetics. 1974; (1): 81-7.
14. Li W, Yang Y, Liu Z-H, Zhao Y-J, et al. Progression of mental health services during the COVID-19 outbreak in China. International journal of biological sciences. 2020; 16(10): 1732.
15. Liu S, Yang L, Zhang C, Xiang Y-T, Liu Z, et al. Online mental health services in China during the COVID-19 outbreak. The Lancet Psychiatry. 2020; 7(4): e17-e8.
16. Lee AM, Wong JG, McAlonan GM, Cheung V, Cheung C, et al. Stress and psychological distress among SARS survivors 1 year after the outbreak. Can J Psychiatry. 2007; 52(4): 233-40.
17. Lai J; Ma S,; Wang Y; et al. Factors Associated With Mental Health Outcomes Among Health Care Workers Exposed to Coronavirus Disease 2019. 2020;3(3):e203976. doi:10.1001/jamanetworkopen.2020.3976
18. Malta M, Rimoin AW, Strathdee SA. The coronavirus 2019-nCoV epidemic: Is hindsight 20/20. EClinicalMedicine. 2020; 1: 20-24. 7
19. Park SC, Park YC. Mental Health Care Measures in Response to the 2019 Novel Coronavirus Outbreak in Korea. Psychiatry Investigation. 2020; 17(2): 85- 91.
20. Fakari FR, Simbar M. Coronavirus Pandemic and Worries during Pregnancy; a Letter to Editor. Archives of Academic Emergency Medicine. 2020; 8(1): 21.
Full-Text: (71 Views)
| Explaining the Factors Involved in Psychological Effects of Covid-19 on Health Care Workers by Interpretive Structural Modeling |
Mohammad Ziaadini1 , Mohammad SadeghAbolhasani1* , Homa Khazaee2 ,
Mohammad Zarezadeh2 , Sedigheh Asadi2 , Farzaneh Ghorbani2 , ElahehSalarikhah2
Mohammad Zarezadeh2
- Department of Management, Rafsanjan Branch, Islamic Azad University, Rafsanjan, Iran
- ShahidSadoughi University of Medical Sciences, Yazd, Iran
| ARTICLE INFO | ABSTRACT | |
| Original Article
Received: 20 April 2022
Accepted: 1 November 2022 |
Background: Spread of COVID-19 worldwide created anxiety, stress. In the meantime, healthcare workers have been suffering from significant psychological distress due to providing direct care to the patient, side injuries and quarantine. The present research aims to investigate and identify the factors involved in reduction of psychological effects of COVID-19 by interpretive structural modeling.
Methods: This study was a mixed study (quantitative and qualitative). The study population included doctors, supervisors and nurses of the clinical departments of Khatam-ul-AnbiyaAbarkoh Hospital in Yazd. The participants were selected using the snowball sampling method. Semi-structured interviews were used to collect data. In the qualitative part of the research, mainly library studies and expert opinions were used. In the quantitative part of the research, the structural self-interaction matrix was used. The final analysis was performed by MATLAB2018. Results: The results show that the most psychological effects of Covid-19 are related to "appropriate measures to reduce the disease such as environmental ventilation" and "financial support of personnel" and "sufficient provision of personal protective equipment" and "dedicated sufficient manpower to the involved departments" (with a power of 8). And the lowest influence is related to "continuous training of stress management and constant presence of a psychologist" (with an influence of influence 5)
Conclusion: The basic factors in the research model include continuous stress management training, the presence of a psychologist, and inspection of infected areas. By the management team and providing adequate personal protective equipment. Keywords: covid-19, mental health, psychological effects |
|
|
Corresponding Author:
Mohammad SadeghAbolhasani Mziaaddini@yahoo.com |
ZiaadiniM, AbolhasaniMS, KhazaeeH, ZarezadehM, AsadiS, Ghorbani F, et al. Explaining the Factors Involved in Psychological Effects of Covid-19 on Healthcare Workers by Interpretive Structural Modeling. J Community Health Research 2023; 12(1): 7-17.
Introduction
In the late 2019, a viral pandemic was reported in Wuhan, China. The disease was caused by a new mutated virus belonging to the coronavirus family called COVID-19 (1). Currently, coronavirus has caused severe and acute respiratory distress syndrome in some patients, and can cause death in some cases. It has spread to all countries all over the world (2). According to the formal reports, more than 128 million people in the world have become infected by March 2021 and the death rate has been reported more than 2.5. The death rate has been reported more than 2.5 million people. In Iran,lackof treatment or prevention ways and the predicted infection of at least 60% of the society suggested by the epidemiologists have created a lot of concern (3). Regarding the pandemic nature of the disease affecting all the economic, political, social, and even military sectors of countries, the psychological effects of this virus on people’s mental health have become significantly important (4). The pathogenic nature of this virus, its quick spread, and death rate, impacts mental health of different classes of the society including patients, healthcare workers, families, children, students, patients with mental illnesses, and even people with different jobs (5- 7). In the face of this large-scale public infectious event, medical workers are under both physical and psychological pressure (6).Stress is an unavoidable phenomenon in life. However, in the case of its repetitive occurrence and the person’s inability to cope with that, it can cause physical and mental disorders (8, 9). Since healthcare workers work in the front line of fighting with this virus, they are more exposed to continuous stress. A paper released in March 2020 titled “The emotional effects of coronavirus” suggests that the elderly with psychiatric disorders are more susceptible to the subsequent distresses. Meanwhile, this paper has shown that most healthcare workers in hospitals do not receive any education for mental health care. Fear is an obvious consequence of social quarantine (10). Based on the results of previous studies obtained at the time of the spread of SARS and Ebola, health care workers suffer from some harmful psychological disorders such as anxiety, fear and stress.Thiscan affect the quality of their activities and services (11).
Another study titled “Immediate psychological responses and correlated factors in the early stages of coronavirus pandemic in Chinese population” has evaluated people’s perception of stress, anxiety, depression, and their related psychological factors in coronavirus pandemic. The people’s psychological impacts and mental health were also evaluated. In this study, 53.8% of the participants reported the experience of moderate to severe psychological impacts of coronavirus, and 16.5% reported moderate to severe depression symptoms. 28.8% reported moderate to severe anxiety symptoms, and 8.1% reported moderate to severe stress. There was a correlation between high levels of psychological impacts of coronavirus, stress, anxiety, depression and female gender, being a student, physical symptoms such as tiredness, dizziness, runny nose, and poor health. Also, there was a correlation between lower levels of psychological impacts of coronavirus, stress, anxiety, and depression and having updated information about treatment methods, pandemic conditions, and prevention means such as washing hands, wearing gloves, and wearing a mask (12).
The initial reachability matrix is obtained by changing the SSIM indicators into zero and one. This matrix only includes zero and one. The zero and one numbers are placed based on the following rules.
-If the cell indicator is V, that cell is assigned 1 and its symmetric cell is assigned 0.
-If the cell indicator is A, that cell is assigned 0 and its symmetric cell is assigned 1.
-If the cell indicator is X, that cell is assigned 1 and its symmetric cell is assigned 1.
-If the cell indicator is O, that cell is assigned 0 and its symmetric cell is assigned 0.
Final reachability matrix
Another study titled “Immediate psychological responses and correlated factors in the early stages of coronavirus pandemic in Chinese population” has evaluated people’s perception of stress, anxiety, depression, and their related psychological factors in coronavirus pandemic. The people’s psychological impacts and mental health were also evaluated. In this study, 53.8% of the participants reported the experience of moderate to severe psychological impacts of coronavirus, and 16.5% reported moderate to severe depression symptoms. 28.8% reported moderate to severe anxiety symptoms, and 8.1% reported moderate to severe stress. There was a correlation between high levels of psychological impacts of coronavirus, stress, anxiety, depression and female gender, being a student, physical symptoms such as tiredness, dizziness, runny nose, and poor health. Also, there was a correlation between lower levels of psychological impacts of coronavirus, stress, anxiety, and depression and having updated information about treatment methods, pandemic conditions, and prevention means such as washing hands, wearing gloves, and wearing a mask (12).
To segment the criteria in the final reachability matrix, driving power and dependence power should be calculated for each of the elements. The driving power of an element refers to the number of criteria that are affected by that element including itself. The dependence power refers to the number of criteria that affect the element and lead to that. The driving and dependence powers are used in the analysis of the Impact Matrix Cross-Reference Multiplication Applied to a Classification (MICMAC) in which the criteria are divided into four groups including autonomous, dependent, linkage, and independent (the driving) criteria. The analysis of Impact Matrix Cross-Reference Multiplication Applied to a Classification (MICMAC) aims to determine the driving and dependence power of the variable.
- The first group includes the autonomous variables that have a poor driving and dependence power. These variables are almost detached from the system and they have weak relationships with that.
- The second group includes the dependent variables that have a poor driving power and a stronger dependence power than the other obstacles.
- The third group includes the linkage variables that have a strong driving and dependence power. These variables are unstable factors; i.e. any action concerning these factors can affect both the factor itself and the other factors.
- The fourth group includes the independent factors that have a strong driving power and a weak dependence power. As it is observed, a criterion with a strong driving power is called the key criterion and is assigned to the group of independent or linkage variables.
The initial reachability matrix is obtained by changing the SSIM indicators into zero and one. This matrix only includes zero and one. The zero and one numbers are placed based on the following rules.
-If the cell indicator is V, that cell is assigned 1 and its symmetric cell is assigned 0.
-If the cell indicator is A, that cell is assigned 0 and its symmetric cell is assigned 1.
-If the cell indicator is X, that cell is assigned 1 and its symmetric cell is assigned 1.
-If the cell indicator is O, that cell is assigned 0 and its symmetric cell is assigned 0.
Final reachability matrix
After developing the initial reachability matrix, the final reachability matrix is formed to adjust the initial reachability matrix. This matrix presents the driving and dependence power of each variable. The driving power of an element refers to the number of criteria that are affected by that element including itself. The dependence power refers to the final number of the variables that create the mentioned variable.
Drawing the model of the interaction of the factor
First, authors put the criteria in a descending order based on their levels. The structural model was drawn by nodes and lines. It was done using the matrix resulted from the ordered matrix. If there was relationship from i to j, it was presented by an arrow from i to j. The final diagram obtained by removing the extended modes and segmentation of the levels is presented in the diagram.
Results
The experts in this research included 30 doctors, supervisors and nurses from the clinical departments of Khatam Hospital with at least 8 years of service experience. Their demographic status is listed in the table below.
The results obtained from the interviews with experts and the use of the interpretive structural method, respectively, with the formation of an interactive structural matrix, are described in the following tables.
The results obtained from the interviews with experts and the use of the interpretive structural method, respectively, with the formation of an interactive structural matrix, are described in the following tables.
Due to the prevalence of COVID-19 disease worldwide and the rate of deaths due to this disease, healthcare workers are more likely than others to be exposed to psychological disorders and anxiety. Based on the results of the presented studies, it seems that the care and maintenance of mental health of medical care workers dealing with infectious patients as well as Covid-19 disease is of great importance.
In this study, in order to level and establish conceptual relationships between the factors affecting the psychological effects of Covid-19 disease among the treatment staff, interpretive structural modeling was used. Interpretive structural modeling is a way to design a pattern of complex and multiple relationships between variables of a phenomenon. Structural-interpretive modeling is one of the exploratory methods of model design in management. In this method, first, effective and basic factors are identified and then, using the method that has been presented, the relationships between these factors and the way to achieve progress by these factors are presented. The ISM method analyses the relationship between indicators by analyzing the criteria at several different levels.
In this study, in order to level and establish conceptual relationships between the factors affecting the psychological effects of Covid-19 disease among the treatment staff, interpretive structural modeling was used. Interpretive structural modeling is a way to design a pattern of complex and multiple relationships between variables of a phenomenon. Structural-interpretive modeling is one of the exploratory methods of model design in management. In this method, first, effective and basic factors are identified and then, using the method that has been presented, the relationships between these factors and the way to achieve progress by these factors are presented. The ISM method analyses the relationship between indicators by analyzing the criteria at several different levels.
The current risky condition has affected mental health of healthcare workers and their psychological wellbeing. Therefore, the present research aims to explaining the factors involved in the psychological effects of covid-19 on healthcare workers. It proposes different plans and protocols to protect their health as well.
Methods
In terms of the type of research, the type of research is mixed (quantitative and qualitative). The statistical population of this research was hospital experts, 30 of whom were selected as a statistical sample using the snowball sampling method. In the qualitative part of the research, mainly library studies and expert opinions were used. In the quantitative part of the research, a structured self-interaction matrix was used. The basis of our pairwise comparisons between research components was used in the form of a square matrix to receive experts' votes and opinions. This research is a descriptive analytical study performed by structural equation modeling. This research has been performed by structural equation modeling SSIM is a systematic method used for developing and understanding the relationships between the elements of a complex system. It was proposed by Warfield in 1974 (13). This method is an interactional learning process in which, a set of different interrelated elements are organized in a comprehensive systematic model. This method helps to develop and direct the complex relationships between the elements of a system. Structural equation modeling primarily provides a list of the variables that are related to the problem. These variables are obtained by studying the literature, expert interview, or questionnaire. This method is an interpretive one, because the judgment of a group of people determines whether there is any relationship between these elements or not. Furthermore, this is a structural method; because the relationships are based on an overall structure derived from a complex set of variables (the main idea of structural equation modeling is to decompose a complex system into several subsystems (elements) by using scientific experience and knowledge of the experts to develop a multilevel structural model.
Structural self-interaction matrix (SSIM)
Structural equation modeling suggests that the experts’ opinions become used in the development of content relationships between the variables based on different management methods such as brainstorming, nominal group, etc. As a result, in this research, the opinions of 30 experts have been used for determining the content relationships between the obstacles to tourism development in Iran. The experts were asked about each pair of criteria to express their opinions about the relationship between the two criteria. Four indicators were used to present the relationships between the two criteria i.e. i and j.
V: If i only affect j. A: If i affects j and j affects i, too.
X: If only j affects i.
O: If there is no relationship between i and j.
According to Warfield instruction (1974) (13), the experts’ opinions were used to determine the relationship between the obstacles to tourism development.
Initial reachability matrix
The structural self-interaction matrix changes into a zero-one matrix that is called the initial reachability matrix. This matrix only includes zero and one. Replacement of zero and one for the four primary numbers (0, -1, 1, and 2) is done as the following:
If the intersection of i and j in SSIM is equal to V, in the reachability matrix (i, j) will be equal to 1 and (j, i) will be equal to 0.
If the intersection of (i, j) in SSIM is equal to A, in the reachability matrix both (i, j) and (j, i) will be equal to 1.
If the intersection of (i, j) in SSIM is equal to X, in the reachability matrix both (i, j) and (j, i) will be equal to 0.
If the intersection of (i, j) in SSIM is equal to O, in the reachability matrix (i, j) will be equal to 0 and (j, i) will be equal to 1.
In matrix D i.e. the initial reachability matrix, zero and one are replaced for each of the dij indicators, while cj indicates the factors involved in reduction of the mental pressure imposed by coronavirus conditions.
Final reachability matrix
The final reachability matrix is obtained for the criteria regarding the extension relationship to adjust the initial reachability matrix. For this purpose, the initial reachability matrix should be raised to the power of K+1; so that (MK=MK+1). In this way, some of the zero elements will also be changed into one and presented as (1*).
After developing the relation matrix or the initial reachability matrix, the final reachability matrix should be obtained by the following relations (I is the identity matrix).
M=D+IAfter developing the relation matrix or the initial reachability matrix, the final reachability matrix should be obtained by the following relations (I is the identity matrix).
M*=MK=MK+1
In large and complex systems, it is assumed that each component can be resulted from itself. So, all the entries of the main diagonal of the final system matrix are always 1. For this purpose, the identity matrix is summed with the initial reachability matrix to get the final matrix. The properties of the final matrix include the following:
M2=M
For this purpose, the obtained final matrix is raised to the power as far as the above situation is realized. Then, the obtained matrix will be the final matrix. The number of 1s located in the first row indicates the lines or the effects on the first criterion. The component that affects all the components of the system and is not affected by any component is called the source.
Stratification of the criteria
After determining the initial and final reachability sets for each of the criteria and determining the joint sets, the criteria will be stratified. The joint set is obtained by finding the commonalities of the initial and final reachability sets. The criteria whose joint set is the same as their reachable set are prioritized as the first level. Other levels of the criteria will be specified by removing these criteria and repeating this process. Then, based on the determined levels and the final matrix, ISM diagram is drawn. Each level is determined by repeating the following rule (C is the set of criteria).
Clustering the criteria
Table 1. Frequency distribution of demographic variables
| Variables | Frequency | Percent | |
| sex | male | 18 | 60.0 |
| Female | 12 | 40.0 | |
| job type | Doctor | 8 | 26.7 |
| Nurse | 12 | 40.0 | |
| Superintendent/ Supervisor | 10 | 33.3 | |
| work experience | N | Mean | Std 4.61 |
| 30 | 11.73 |
Table 2. Structural self-interaction matrix
| j i |
C1 | C2 | C3 | C4 | C5 | C6 | C7 | C8 | |
| C1 | Adopting proper Strategies to reduce the transmission of disease, for example using ventilation | - | X | X | A | X | A | O | O |
| C2 | Providing information about COVID-19 and its transmission ways, observance of the protocols | - | V | O | O | O | X | O | |
| C3 | Providing financial support for the personnel | - | O | O | V | X | X | ||
| C4 | Continuous education on stress management and continuous presence of a psychologist | - | X | A | O | O | |||
| C5 | Continuous inspection of the infected wards by the management team | - | A | X | O | ||||
| C6 | Supplying enough personal protective equipment | - | O | X | |||||
| C7 | Allocating enough human force to the infected wards | - | O | ||||||
| C8 | Allocating a space to a virtual contact room for health workers’ communication with their families | - | |||||||
To show a one-way effect (criterion j leads to criterion i) A
To show the two-way influence of X
To show the lack of relationship between the two criteria O
Table 3. Primary access matrix Factors affecting the psychological effects of Covid-19
| j i | C1 | C2 | C3 | C4 | C5 | C6 | C7 | C8 |
| C1 | 1 | 1 | 1 | 0 | 1 | 0 | 0 | 0 |
| C2 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 0 |
| C3 | 1 | 0 | 1 | 0 | 0 | 1 | 1 | 1 |
| C4 | 1 | 0 | 0 | 1 | 1 | 0 | 0 | 0 |
| C5 | 1 | 0 | 0 | 1 | 1 | 0 | 1 | 0 |
| C6 | 1 | 0 | 0 | 1 | 1 | 1 | 0 | 1 |
| C7 | 0 | 1 | 1 | 0 | 1 | 0 | 1 | 0 |
| C8 | 0 | 0 | 1 | 0 | 0 | 1 | 0 | 1 |
- If the symbol of the house is v, the number one is placed in that house and the number zero is placed in the corresponding house.
- If the house symbol is A, the number zero is placed in that house and the number one is placed in the corresponding house.
- If the symbol of the house is x, the number one is placed in that house and the number one is placed in the corresponding house.
- If the symbol of the house is o, the number zero is placed in that house and the number zero is placed in the corresponding house.
- If the house symbol is A, the number zero is placed in that house and the number one is placed in the corresponding house.
- If the symbol of the house is x, the number one is placed in that house and the number one is placed in the corresponding house.
- If the symbol of the house is o, the number zero is placed in that house and the number zero is placed in the corresponding house.
Table 4. The ultimate access matrix Factors affecting the psychological effects of Covid-19
| j i |
C1 | C2 | C3 | C4 | C5 | C6 | C7 | C8 | Penetration power |
| C1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 |
| C2 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 7 |
| C3 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 |
| C4 | 0 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 5 |
| C5 | 0 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 6 |
| C6 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 |
| C7 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 |
| C8 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 7 |
| The degree of dependence | 8 | 7 | 8 | 7 | 7 | 6 | 8 | 6 |
The results show that the strongest effect is that of “adopting proper strategies to reduce the transmission of the disease, for example using ventilation”, “providing financial support for the personnel”, “supplying adequate personal protective equipment”, and “allocating adequate human force to the infected wards” (with the Penetration power of 8) and the weakest driving power is that of “continuous education of stress management and continuous presence of a psychologist” (with the Penetration power of 5).
Table 5. The level of variables of the psychological effects of Covid-19
| No | Factors affecting the psychological effects of Covid-19 | Leveling criteria |
| 1 | Adopting proper strategies to reduce transmission of the disease, for example using ventilation | 1 |
| 2 | Providing information about COVID-19 and its transmission ways, observing protocols | 2 |
| 3 | Providing financial support for personnel | 1 |
| 4 | Continuous education on stress management and continuous presence of a psychologist | 3 |
| 5 | Continuous inspection of the infected wards by the management team | 3 |
| 6 | Supplying enough personal protective equipment | 3 |
| 7 | Allocating adequate human force to the infected wards | 1 |
| 8 | Allocating a space to a virtual contact room for the health workers’ communication with their families | 2 |
In order to determine the level of factors in the final model, for each of them, access to the set of prerequisites and subscriptions is determined. The access set, in addition to the agent itself, includes the set of factors that the investigated agent leads to. The access set is a prerequisite. If the set of access and sharing is the same for an agent, that agent is placed at the highest level, then this agent is leveled, set aside, and the leveling for other agents continues in the same way until all agents are leveled. The result leads to the definition of 3 levels.

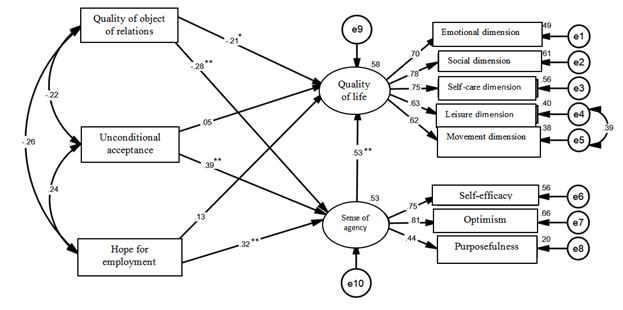
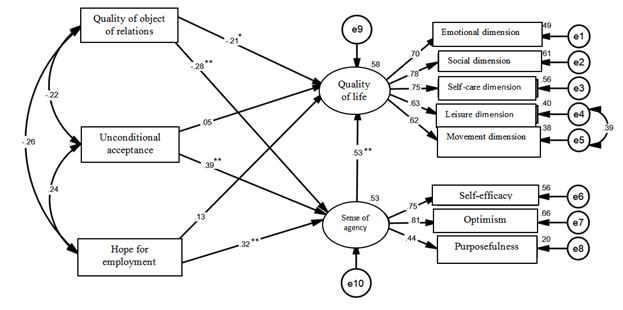
Shape 1. Model of mutual effects of psychological effects of covid19
The first level was determined as the mostly affected group and the last level was determined as the most effective group. As seen in the figure, the third level factors (continuous education of stress management and continuous presence of a psychologist, continuous inspection of the infected wards by the management team, and supplying adequate personal protective equipment) are the fundamental factors of the research model. As a result, the factors involved in reduction of the mental atmosphere and the dominating conditions should originate from the mentioned variables and generalized to other variables. The second-level factors that affect the first-level factors include promotion of information about coronavirus and its transmission ways, observance of the protocols, and allocating a space to virtual contact room for the health care workers to communicate with their families. The first-level factors (assigning adequate human force to infected wards, providing financial support for the personnel, and adopting appropriate strategies to reduce the viral transmission such as ventilation) are mutually interdependent and they do not affect the other factors by themselves.
Table 6. Power of influence and dependence Factors of the psychological effects of Covid-19
| C1 | C2 | C3 | C4 | C5 | C6 | C7 | C8 | |
| Penetration power | 8 | 7 | 8 | 5 | 6 | 8 | 8 | 7 |
| The power of dependence | 8 | 7 | 8 | 7 | 7 | 6 | 8 | 6 |
After determining Penetration and dependence powers, by MICMAC analysis that presents the Penetration and dependence power of the variables, researchers included all the factors in the four clusters of Impact Matrix Cross-Reference Multiplication Applied to a Classification (MICMAC). On the developed MICMAC matrix, the border points are usually larger than the average number of factors by one unit. In other words, since eight factors are studied in this research, the number of border points on the MICMAC matrix was considered 5. However, regarding the research conditions, different borders can be also considered. The borders should be determined so that they can well classify the factors into the clusters. In figure 5, the horizontal axis presents the dependence power, and the vertical axis presents the driving power.
Discussion
After the spread of the corona virus, nurses and doctors were at the forefront of fighting this virus, after the announcement of the pandemic situation in the world, fear and anxiety increased among all the people of the world as well as the medical staff. It was named as the most common mental disorders among the therapy staff.
In this article, we tried to introduce the importance and explain the psychological effects of the covid-19 disease among the employees. For this purpose, in order to identify the effective factors in reducing the psychological effects, the literature review and the opinions of the identified experts were used, and finally, by using the interpretative structure modeling technique, the experts' opinions and their connection and sequence were integrated. Known effective factors include adopting appropriate measures to reduce disease transmission, such as environmental ventilation, increasing information about corona and the ways of transmission and compliance with protocols, financial support of personnel, Continuous training of stress management and permanent presence of a psychologist, continuous visits of the management team to the involved departments, provision of sufficient personal protective equipment, allocation of sufficient manpower for the involved departments, allocation of a space as a virtual room for communication with the family, which was extracted using MICMAC analysis, which diagnosed And the analysis shows the power of influence and dependence of the variables, and after determining the power of influence or influence and the power of dependence, all the factors can be placed in the four clusters of the applied cross-reference multiplication effect matrix method.
In this article, we tried to introduce the importance and explain the psychological effects of the covid-19 disease among the employees. For this purpose, in order to identify the effective factors in reducing the psychological effects, the literature review and the opinions of the identified experts were used, and finally, by using the interpretative structure modeling technique, the experts' opinions and their connection and sequence were integrated. Known effective factors include adopting appropriate measures to reduce disease transmission, such as environmental ventilation, increasing information about corona and the ways of transmission and compliance with protocols, financial support of personnel, Continuous training of stress management and permanent presence of a psychologist, continuous visits of the management team to the involved departments, provision of sufficient personal protective equipment, allocation of sufficient manpower for the involved departments, allocation of a space as a virtual room for communication with the family, which was extracted using MICMAC analysis, which diagnosed And the analysis shows the power of influence and dependence of the variables, and after determining the power of influence or influence and the power of dependence, all the factors can be placed in the four clusters of the applied cross-reference multiplication effect matrix method.
According to MICMAC analysis, “continuous education on stress management and continuous presence of a psychologist” has been the most affected factors. They are, therefore, considered dependence factors with poor driving power. Nevertheless, they have a higher dependence power than other factors. In other words, these factors are the result of interactions between other factors. In fact, there are more important factors involved in reduction of the mental pressure of COVID-19 leading to this factor.
Other variables are considered linkage variables; i.e. they have strong driving power and dependence power. Those with high driving power are considered the key variables. They belong to the independent or linkage groups. Any action concerning these variables leads to a change in other variables. Meanwhile, no variable belonged to the autonomous and independent groups.
Zhan et al. confirmed that the stress caused by the fear of COVID-19 in a two-way relationship with physical infections leads to a decrease in health, sleep quality and post-traumatic stress symptoms. This is due to the effects of COVID-19 stress on the subscale of anxiety symptoms and disorder. Sleep regards the health of the same people, which in this study, the relationship equals to 31(19). Shigemura et al. demonstrated that using coping skills to control stress causes many problems in the field of mental health. The rapid spread of the Covid-19 and the crisis caused by this virus and the current high-risk mental health status of individuals and especially the medical staff is endangered (20). Therefore, identifying the cause of these psychological disorders in the medical staff, whose mental health may be endangered, is essential in order to maintain the mental health of individuals. This is done using appropriate psychotherapy methods.
In this regard, China uses the Internet to screen and identify people prone to psychological disorders and develop self-help protocols for general public. The protocols are also for special groups such as children of pregnant women, the elderly, and people who have lost loved ones due to the disease and the staff (14). China has also used several artificial intelligence programs to intervene in the psychological crises caused by the COVID-19 pandemic (15).Previous studies during the Sars epidemic in 2003 showed that medical staffs were afraid of family, friends and colleagues getting infected. Often the staffs felt sick and therefore were reluctant to work and had high levels of stress symptoms. They reported depression. These problems can have long-term psychological consequences (16)
Other variables are considered linkage variables; i.e. they have strong driving power and dependence power. Those with high driving power are considered the key variables. They belong to the independent or linkage groups. Any action concerning these variables leads to a change in other variables. Meanwhile, no variable belonged to the autonomous and independent groups.
Zhan et al. confirmed that the stress caused by the fear of COVID-19 in a two-way relationship with physical infections leads to a decrease in health, sleep quality and post-traumatic stress symptoms. This is due to the effects of COVID-19 stress on the subscale of anxiety symptoms and disorder. Sleep regards the health of the same people, which in this study, the relationship equals to 31(19). Shigemura et al. demonstrated that using coping skills to control stress causes many problems in the field of mental health. The rapid spread of the Covid-19 and the crisis caused by this virus and the current high-risk mental health status of individuals and especially the medical staff is endangered (20). Therefore, identifying the cause of these psychological disorders in the medical staff, whose mental health may be endangered, is essential in order to maintain the mental health of individuals. This is done using appropriate psychotherapy methods.
In this regard, China uses the Internet to screen and identify people prone to psychological disorders and develop self-help protocols for general public. The protocols are also for special groups such as children of pregnant women, the elderly, and people who have lost loved ones due to the disease and the staff (14). China has also used several artificial intelligence programs to intervene in the psychological crises caused by the COVID-19 pandemic (15).Previous studies during the Sars epidemic in 2003 showed that medical staffs were afraid of family, friends and colleagues getting infected. Often the staffs felt sick and therefore were reluctant to work and had high levels of stress symptoms. They reported depression. These problems can have long-term psychological consequences (16)
The results of this study are consistent with the findings of Lai et al.'s 2020 study (17). This study was based on the survey of the mental health results of 1257 health care workers in 34 hospitals serving corona patients. This study showed that the covid-19 virus has had psychological effects on the medical staff of hospital centers, especially nurses, which makes the need for a comprehensive study even more obvious. Treatment staff direct involvement with this disease and the risks of transmission of this disease, the medical staff must be continuously present in the work environment and are deprived of visiting their families. Therefore, it is not surprising that the mental health of healthcare workers is at risk. Paying attention to stress management strategies and taking appropriate measures in this regard is as important as maintaining the physical health of the personnel (18).
Although this research is theoretically based on the choice of the subject is an innovation, but there were some limitations. This study was conducted only on the medical staff of Khatam Al-Abiai Abarkooh Hospital. So, it was not possible to generalize the results to other geographical areas. One of the strengths of this study was providing solutions to reduce the psychological effects of this virus on the medical staff and encourage managers and policymakers to take appropriate intervention measures.
Although this research is theoretically based on the choice of the subject is an innovation, but there were some limitations. This study was conducted only on the medical staff of Khatam Al-Abiai Abarkooh Hospital. So, it was not possible to generalize the results to other geographical areas. One of the strengths of this study was providing solutions to reduce the psychological effects of this virus on the medical staff and encourage managers and policymakers to take appropriate intervention measures.
Conclusion
The results of the current research show that by identifying effective factors in reducing psychological effects, including adopting appropriate measures to reduce disease transmission, including environmental ventilation. Increasing information about the corona virus and ways of transmission and compliance with protocols Financial support for personnel Continuous education of stress management and continuous presence of a psychologist Continuous visit of the management team to the involved departments Provision of adequate personal protective equipment Allocation of sufficient manpower for the departments involved Allocating a space as a virtual room to communicate with the family And the effective implementation of these factors can play an effective role by reducing the psychological burden of people. In the fight against this virus, managers and policy makers played a role and helped to maintain the mental health of the medical staff.
Acknowledgement
This study obtained ethics approval (Code: IR.SSU.SPH.REC.1401.167) from Faculty of Health Shahid Sadougi University of Medical Sciences, Yazd.
Conflict of interest
The authors declare that there are no conflicts there are no interests in the present study.
Authors’ contribution
This study obtained ethics approval (Code: IR.SSU.SPH.REC.1401.167) from Faculty of Health Shahid Sadougi University of Medical Sciences, Yazd.
Conflict of interest
The authors declare that there are no conflicts there are no interests in the present study.
Authors’ contribution
MS.A, M.Z, Conceived and designed the analysis: Data collection E.S, F.GH, S.A Data analysis: H.KH.Drafting of the manuscript:MS.A.All authors contributed to and reviewed the final version of the manuscript. All the authors met the criteria of authorship based on the recommendations of the international committee of medical journal editors.
References
1. Shigemura J, Ursano RJ, Morganstein JC, Kurosawa M, Benedek DM. Public responses to the novel 2019 coronavirus (2019‐nCoV) in Japan: Mental health consequences and target populations. Psychiatry and clinical neurosciences. 2020; 74(4): 281.
2. Zhang F, Shang Z, Ma H, Jia Y, Sun L, et al. High risk of infection caused posttraumatic stress symptoms in individuals with poor sleep quality: A study on influence of coronavirus disease (COVID-19) in China. MedRxiv. 2020.
3. Lai C-C, Shih T-P, Ko W-C, Tang H-J, Hsueh P-R. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease-2019 (COVID-19): The epidemic and the challenges. International journal of antimicrobial agents. 2020; 55(3): 105924.
4. Li S, Wang Y, Xue J, Zhao N, Zhu T. The impact of COVID-19 epidemic declaration on psychological consequences: a study on active Weibo users. International journal of environmental research and public health. 2020; 17(6): 2032.
5. Bao Y, Sun Y, Meng S, Shi J, Lu L. 2019-nCoV epidemic: address mental health care to empower society. The Lancet. 2020; 395(10224): e37-e8.
6. Chen Q, Liang M, Li Y, Guo J, Fei D, et al. Mental health care for medical staff in China during the COVID-19 outbreak. The Lancet Psychiatry. 2020; 7(4): e15-e6.
7. Xiang Y-T, Yang Y, Li W, Zhang L, Zhang Q, et al. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. The lancet psychiatry. 2020; 7(3): 228-9.
8. Kittrell Chitty K. Professional nursing concepts & challenges. Amsterdam, Netherlands: Elsevier Science Health Science div; 2004.
9. Perry AG, Potter P. Basic nursing: Essentials for practice: Mosby, Elsevier; 2003.
10. Kang L, Li Y, Hu S, Chen M, Yang C, et al. The mental health of medical workers in Wuhan, China dealing with the 2019 novel coronavirus. The Lancet Psychiatry. 2020.
11. Li L, Wan C, Ding R, Liu Y, Chen J, et al. Mental distress among Liberian medical staff working at the China Ebola Treatment Unit: a cross sectional study. Health and quality of life outcomes. 2015; 13(1): 1-6.
12. Huang L, rong Liu H. Emotional responses and coping strategies of nurses and nursing college students during COVID-19 outbreak. MedRxiv. 2020.
13. Warfield JN. Developing interconnection matrices in structural modeling. IEEE Transactions on Systems, Man, and Cybernetics. 1974; (1): 81-7.
14. Li W, Yang Y, Liu Z-H, Zhao Y-J, et al. Progression of mental health services during the COVID-19 outbreak in China. International journal of biological sciences. 2020; 16(10): 1732.
15. Liu S, Yang L, Zhang C, Xiang Y-T, Liu Z, et al. Online mental health services in China during the COVID-19 outbreak. The Lancet Psychiatry. 2020; 7(4): e17-e8.
16. Lee AM, Wong JG, McAlonan GM, Cheung V, Cheung C, et al. Stress and psychological distress among SARS survivors 1 year after the outbreak. Can J Psychiatry. 2007; 52(4): 233-40.
17. Lai J; Ma S,; Wang Y; et al. Factors Associated With Mental Health Outcomes Among Health Care Workers Exposed to Coronavirus Disease 2019. 2020;3(3):e203976. doi:10.1001/jamanetworkopen.2020.3976
18. Malta M, Rimoin AW, Strathdee SA. The coronavirus 2019-nCoV epidemic: Is hindsight 20/20. EClinicalMedicine. 2020; 1: 20-24. 7
19. Park SC, Park YC. Mental Health Care Measures in Response to the 2019 Novel Coronavirus Outbreak in Korea. Psychiatry Investigation. 2020; 17(2): 85- 91.
20. Fakari FR, Simbar M. Coronavirus Pandemic and Worries during Pregnancy; a Letter to Editor. Archives of Academic Emergency Medicine. 2020; 8(1): 21.
Review: Research |
Subject:
Public Health
Received: 2022/04/20 | Accepted: 2022/11/1 | Published: 2023/03/19
Received: 2022/04/20 | Accepted: 2022/11/1 | Published: 2023/03/19
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution 4.0 International License. |





